Volume 12, Issue 2 (June 2025)
Avicenna J Neuro Psycho Physiology 2025, 12(2): 96-102 |
Back to browse issues page
Ethics code: KUMS.REC.1402.590
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mirzaei-Alavijeh M, Moradinazar M, Karimi N, Jalilian F. Childbirth Decisions: How Socio-economic Determinants and Tokophobia Shape Delivery Choices. Avicenna J Neuro Psycho Physiology 2025; 12 (2) :96-102
URL: http://ajnpp.umsha.ac.ir/article-1-529-en.html
URL: http://ajnpp.umsha.ac.ir/article-1-529-en.html
1- Social Development and Health Promotion Research Center, Health Policy and Promotion Research Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
2- Department of Health Education and Promotion, School of Health, Kermanshah University of Medical Sciences, Kermanshah, Iran. ,f_jalilian@yahoo.com
2- Department of Health Education and Promotion, School of Health, Kermanshah University of Medical Sciences, Kermanshah, Iran. ,
Full-Text [PDF 417 kb]
(221 Downloads)
| Abstract (HTML) (832 Views)
Table 3. Linear regression analysis of Tokophobia components based on childbirth history and delivery method
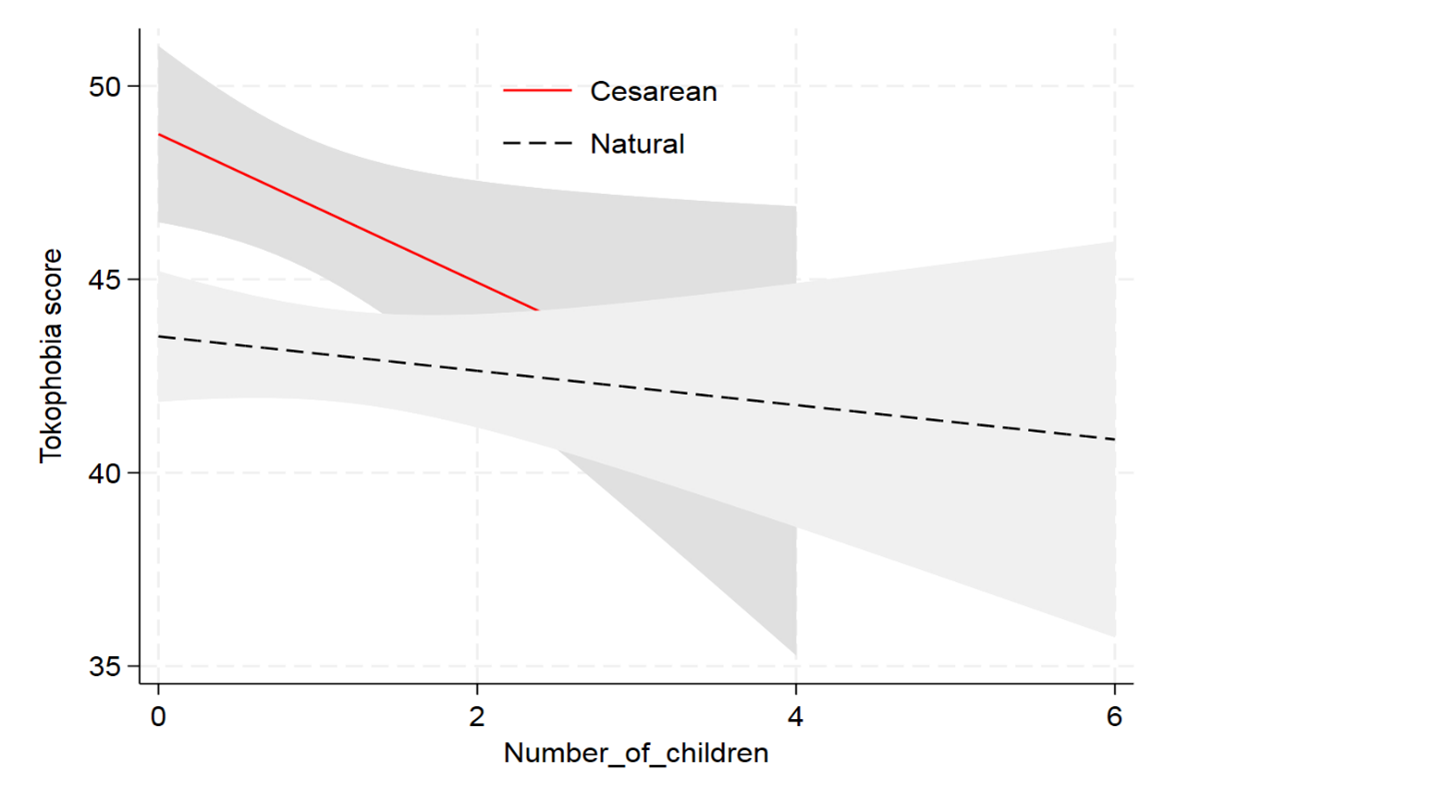
Figure 1. Comparison of Tokophobia scores across childbirth history and delivery methods
Full-Text: (166 Views)
Background
Fear of childbirth, medically known as tokophobia, is a significant psychological concern affecting pregnant women worldwide, with profound implications for maternal mental health and pregnancy outcomes [1]. This fear, which can manifest during various stages of pregnancy and postpartum, not only negatively impacts the childbirth experience but may also lead to physical and psychological complications for both the mother and her family [2]. Research has established a correlation between fear of childbirth and increased use of epidural anesthesia, prolonged labor, a higher risk of labor dystocia, and emergency cesarean sections [3]. A negative childbirth experience can disrupt maternal-infant bonding and reduce exclusive breastfeeding rates [4]. Several factors contribute to the development of tokophobia, including personality traits, such as anxiety, traumatic childbirth experiences, a history of miscarriage, insufficient social support, and poor relationships with a partner [5]. Furthermore, fear and anxiety during labor can lead to increased muscle tension, potentially hindering pelvic expansion during vaginal delivery; this exacerbates pain and perpetuates a cycle of fear, tension, and discomfort [6]. Studies also emphasize that fear of childbirth plays a crucial role in women's decision-making processes, influencing their choices regarding the mode of delivery [2]. The childbirth process presents women with various challenges and risks throughout pregnancy, labor, and the postpartum period; one of the most critical decisions in this journey is the choice of delivery method, which has a significant impact on both maternal and neonatal health; this decision should be made based on a thorough assessment of the mother’s and baby’s condition during pregnancy [7].
Objectives
Decision-making regarding childbirth is shaped by a complex interplay of factors that must be carefully considered to ensure optimal outcomes for both mother and child. The present study aims to investigate the influence of socio-demographic characteristics and prior childbirth experiences on tokophobia among pregnant women in western Iran. Specifically, it explores the associations between delivery method, number of children, history of miscarriage, and educational attainment with childbirth preferences, seeking to identify underlying patterns in women's choices between vaginal and cesarean delivery. Furthermore, the study examines the extent to which the mode of delivery affects the severity of tokophobia symptoms—such as panic responses, social withdrawal, and disruptions to daily functioning. The findings are intended to inform the development of targeted prenatal care strategies and psychological interventions aimed at alleviating childbirth-related fear and enhancing maternal well-being.
Materials and Methods
Study Design and Perspective
This descriptive-analytical study was conducted in 2024 among a sample of 1,001 pregnant women in Kermanshah, Iran. Participants were recruited from a range of healthcare settings, including public health centers, clinics, and private obstetric offices throughout the city. To enhance the representativeness of the sample, a multistage sampling strategy was employed. Initially, Kermanshah was divided into eight municipal districts, each serving as a distinct cluster. Within each cluster, two health centers, two clinics, and two private obstetric offices were randomly selected for the study. Pregnant women who were present and accessible at these facilities during the data collection period were then selected using simple random sampling.
Participants were recruited through direct, face-to-face engagement at selected healthcare facilities and were formally invited to participate in the study. Individuals who provided informed consent and met the inclusion criteria—namely, being currently pregnant and expressing willingness to participate—were administered structured self-report questionnaires. The sole exclusion criterion was the presence of incomplete responses. Following a thorough review, questionnaires deemed substantially incomplete were excluded from the dataset. Ultimately, 992 completed and valid questionnaires were retained for statistical analysis, corresponding to a final response rate of 99.1%.
Questionnaire
The questionnaire used in this study was organized into two main sections, each designed to capture essential information related to participant demographics and the assessment of tokophobia. The first section collected key background data, including age, number of children, history of abortion, educational level, employment status, economic condition, gestational age in the current pregnancy, participation in childbirth education classes, and health insurance coverage. These variables provided a comprehensive overview of the socio-demographic factors potentially influencing childbirth preferences and experiences. The second section assessed tokophobia using a standardized and validated instrument.
Tokophobia was assessed using the Tokophobia Assessment Questionnaire (TAQ), a standardized and validated instrument developed by Nunes et al. in 2020 for use in the Brazilian population. The TAQ comprises 25 items distributed across six conceptual domains: physical summation, feelings of panic, social involvement, interference with daily habits, pregnancy avoidance, and self-perception of tokophobia. It was designed to capture the emotional, psychological, and behavioral dimensions of childbirth-related fear. Each of the six domains includes representative items that reflect the nature of tokophobia. For instance, the physical summation domain includes “My fear of childbirth is causing me physical symptoms,” while the feelings of panic domain features “Just talking about childbirth makes me feel desperate.” The social involvement domain addresses interpersonal impact, such as “My fear of childbirth is interfering with my relationship with my family.” In the domain of interference with daily habits, items, such as “My fear of childbirth is affecting my sleep” illustrate disruptions to routine functioning. The pregnancy avoidance domain includes “I tried to avoid pregnancy as much as possible due to my intense fear of childbirth,” and the self-perception of tokophobia domain captures internal beliefs, exemplified by “I consider childbirth to be extremely dangerous.” The TAQ has demonstrated strong psychometric properties, including a Cronbach’s alpha of 0.935, indicating excellent internal consistency. Reliability was further supported by Pearson and intraclass correlation coefficients, and construct validity was confirmed through exploratory factor analysis. Although originally developed in Portuguese, the TAQ was linguistically adapted for use in our population and retains conceptual relevance across cultural contexts [8]. In the present study, the TAQ was administered as part of a structured self-report survey. Internal consistency was reassessed, and the instrument showed a Cronbach’s alpha of 0.95, confirming its reliability within our sample and supporting its suitability for use in the target population. Higher scores reflect greater tokophobia.
Data Analysis
Data analysis was performed using the SPSS (version 16) software. Both descriptive and inferential statistical methods were employed to assess the socio-demographic influences and variations in tokophobia among participants. Descriptive statistics, including means, standard deviations, and frequency distributions, were used to summarize participant characteristics and childbirth preferences. Chi-square tests were conducted to examine associations between categorical variables, revealing statistically significant relationships between age, number of children, abortion history, education level, and delivery preferences. Furthermore, linear regression analysis was employed to assess the impact of childbirth history and delivery method on tokophobia scores, adjusting for key covariates.
Results
Table 1 highlights significant socio-demographic factors influencing delivery preferences, including age, number of children, abortion history, and educational level. Age demonstrates a strong statistical association (P<0.001), with younger women (≤20 years) showing a higher probability of cesarean deliveries, while older age groups, particularly women aged 31-39 and ≥40, are more likely to opt for natural births. Similarly, the number of children shows a significant link (P<0.001), as women without children predominantly favor cesarean sections, whereas those with three or more children overwhelmingly opt for natural births. Additionally, a history of abortion is significantly associated with delivery preferences (P<0.001), with women who have had an abortion more likely to choose natural births.
Educational attainment and employment status also play meaningful roles (P < 0.001 for both). Women with primary or secondary education tend to prefer cesarean deliveries, whereas those with higher education show a greater inclination toward natural childbirth. Similarly, housewives are more likely to choose cesareans, while employed women lean towards natural births. Participation in childbirth classes (P=0.014) correlates strongly with higher natural birth rates.
Objectives
Decision-making regarding childbirth is shaped by a complex interplay of factors that must be carefully considered to ensure optimal outcomes for both mother and child. The present study aims to investigate the influence of socio-demographic characteristics and prior childbirth experiences on tokophobia among pregnant women in western Iran. Specifically, it explores the associations between delivery method, number of children, history of miscarriage, and educational attainment with childbirth preferences, seeking to identify underlying patterns in women's choices between vaginal and cesarean delivery. Furthermore, the study examines the extent to which the mode of delivery affects the severity of tokophobia symptoms—such as panic responses, social withdrawal, and disruptions to daily functioning. The findings are intended to inform the development of targeted prenatal care strategies and psychological interventions aimed at alleviating childbirth-related fear and enhancing maternal well-being.
Materials and Methods
Study Design and Perspective
This descriptive-analytical study was conducted in 2024 among a sample of 1,001 pregnant women in Kermanshah, Iran. Participants were recruited from a range of healthcare settings, including public health centers, clinics, and private obstetric offices throughout the city. To enhance the representativeness of the sample, a multistage sampling strategy was employed. Initially, Kermanshah was divided into eight municipal districts, each serving as a distinct cluster. Within each cluster, two health centers, two clinics, and two private obstetric offices were randomly selected for the study. Pregnant women who were present and accessible at these facilities during the data collection period were then selected using simple random sampling.
Participants were recruited through direct, face-to-face engagement at selected healthcare facilities and were formally invited to participate in the study. Individuals who provided informed consent and met the inclusion criteria—namely, being currently pregnant and expressing willingness to participate—were administered structured self-report questionnaires. The sole exclusion criterion was the presence of incomplete responses. Following a thorough review, questionnaires deemed substantially incomplete were excluded from the dataset. Ultimately, 992 completed and valid questionnaires were retained for statistical analysis, corresponding to a final response rate of 99.1%.
Questionnaire
The questionnaire used in this study was organized into two main sections, each designed to capture essential information related to participant demographics and the assessment of tokophobia. The first section collected key background data, including age, number of children, history of abortion, educational level, employment status, economic condition, gestational age in the current pregnancy, participation in childbirth education classes, and health insurance coverage. These variables provided a comprehensive overview of the socio-demographic factors potentially influencing childbirth preferences and experiences. The second section assessed tokophobia using a standardized and validated instrument.
Tokophobia was assessed using the Tokophobia Assessment Questionnaire (TAQ), a standardized and validated instrument developed by Nunes et al. in 2020 for use in the Brazilian population. The TAQ comprises 25 items distributed across six conceptual domains: physical summation, feelings of panic, social involvement, interference with daily habits, pregnancy avoidance, and self-perception of tokophobia. It was designed to capture the emotional, psychological, and behavioral dimensions of childbirth-related fear. Each of the six domains includes representative items that reflect the nature of tokophobia. For instance, the physical summation domain includes “My fear of childbirth is causing me physical symptoms,” while the feelings of panic domain features “Just talking about childbirth makes me feel desperate.” The social involvement domain addresses interpersonal impact, such as “My fear of childbirth is interfering with my relationship with my family.” In the domain of interference with daily habits, items, such as “My fear of childbirth is affecting my sleep” illustrate disruptions to routine functioning. The pregnancy avoidance domain includes “I tried to avoid pregnancy as much as possible due to my intense fear of childbirth,” and the self-perception of tokophobia domain captures internal beliefs, exemplified by “I consider childbirth to be extremely dangerous.” The TAQ has demonstrated strong psychometric properties, including a Cronbach’s alpha of 0.935, indicating excellent internal consistency. Reliability was further supported by Pearson and intraclass correlation coefficients, and construct validity was confirmed through exploratory factor analysis. Although originally developed in Portuguese, the TAQ was linguistically adapted for use in our population and retains conceptual relevance across cultural contexts [8]. In the present study, the TAQ was administered as part of a structured self-report survey. Internal consistency was reassessed, and the instrument showed a Cronbach’s alpha of 0.95, confirming its reliability within our sample and supporting its suitability for use in the target population. Higher scores reflect greater tokophobia.
Data Analysis
Data analysis was performed using the SPSS (version 16) software. Both descriptive and inferential statistical methods were employed to assess the socio-demographic influences and variations in tokophobia among participants. Descriptive statistics, including means, standard deviations, and frequency distributions, were used to summarize participant characteristics and childbirth preferences. Chi-square tests were conducted to examine associations between categorical variables, revealing statistically significant relationships between age, number of children, abortion history, education level, and delivery preferences. Furthermore, linear regression analysis was employed to assess the impact of childbirth history and delivery method on tokophobia scores, adjusting for key covariates.
Results
Table 1 highlights significant socio-demographic factors influencing delivery preferences, including age, number of children, abortion history, and educational level. Age demonstrates a strong statistical association (P<0.001), with younger women (≤20 years) showing a higher probability of cesarean deliveries, while older age groups, particularly women aged 31-39 and ≥40, are more likely to opt for natural births. Similarly, the number of children shows a significant link (P<0.001), as women without children predominantly favor cesarean sections, whereas those with three or more children overwhelmingly opt for natural births. Additionally, a history of abortion is significantly associated with delivery preferences (P<0.001), with women who have had an abortion more likely to choose natural births.
Educational attainment and employment status also play meaningful roles (P < 0.001 for both). Women with primary or secondary education tend to prefer cesarean deliveries, whereas those with higher education show a greater inclination toward natural childbirth. Similarly, housewives are more likely to choose cesareans, while employed women lean towards natural births. Participation in childbirth classes (P=0.014) correlates strongly with higher natural birth rates.
| Variable | Total N (%) | Do you have a history of childbirth? | P-value | ||||
| Yes | No | ||||||
| Natural | Cesarean | Probability Natural | Probability Cesarean | ||||
| Age | 20≥ | 147 (14.84%) | 14 (9.52%) | 62 (42.18%) | 18 (12.24%) | 53 (36.05%) | <0.001 |
| 21-29 | 431 (43.48%) | 78 (18.10%) | 121 (28.07%) | 165 (38.28%) | 67 (15.55%) | ||
| 31-39 | 340 (34.29%) | 89 (26.18%) | 44 (12.94%) | 174 (51.18%) | 33 (9.71%) | ||
| 40≤ | 74 (7.47%) | 21 (28.38%) | 3 (4.05%) | 43 (58.11%) | 7 (9.46%) | ||
| Number of Children | No child | 387(39.01) | - | 230 (59.43%) | - | 157 (40.57%) | <0.001 |
| 1-2 | 511(51.51) | 182(35.62) | - | 326(63.80) | 3(0.59) | ||
| 3≤ | 94(9.48) | 20(21.28) | - | 74(78.72) | - | ||
| Abortion | No | 703 (70.77%) | 126 (17.92%) | 183 (26.03%) | 263 (37.41%) | 131 (18.63%) | <0.001 |
| Yes | 237 (29.23%) | 58 (24.47%) | 39 (16.46%) | 115 (48.52%) | 25 (10.55%) | ||
| Education | Primary | 107 (10.87%) | 25 (23.36%) | 11 (10.28%) | 59 (55.14%) | 12 (11.21%) | <0.001 |
| Secondary | 315 (31.84%) | 53 (16.83%) | 93 (29.52%) | 121 (38.41%) | 48 (15.24%) | ||
| Diploma | 339 (34.24%) | 71 (20.94%) | 68 (20.06%) | 151 (44.54%) | 49 (14.45%) | ||
| Academic | 221 (22.05%) | 50 (22.62%) | 57 (25.79%) | 63 (28.51%) | 51 (23.08%) | ||
| Job | Housewife | 773 (78.04%) | 151 (19.53%) | 191 (24.71%) | 324 (41.91%) | 107 (13.84%) | <0.001 |
| Employed | 205 (21.96%) | 44 (21.46%) | 38 (18.54%) | 70 (34.15%) | 53 (25.85%) | ||
| Economic Status | Poor | 186 (18.78%) | 36 (19.35%) | 40 (21.51%) | 78 (41.94%) | 32 (17.20%) | 0.07 |
| Moderate | 673 (68.14%) | 139 (20.65%) | 162 (24.07%) | 277 (41.16%) | 95 (14.12%) | ||
| Good | 128 (12.93%) | 24 (18.75%) | 28 (21.88%) | 43 (33.59%) | 33 (25.78%) | ||
| Health Insurance | No | 247 (25.25%) | 59 (23.89%) | 45 (18.22%) | 104 (42.11%) | 39 (15.79%) | 0.152 |
| Yes | 730 (74.75%) | 141 (19.32%) | 178 (24.38%) | 290 (39.73%) | 121 (16.58%) | ||
| Pregnancy Week for this Childbirth | 10≥ | 163 (17.77%) | 36 (22.09%) | 35 (21.47%) | 60 (36.81%) | 32 (19.63%) | 0.042 |
| 11-29 | 518 (56.55%) | 110 (21.24%) | 101 (19.50%) | 216 (41.70%) | 91 (17.57%) | ||
| 30≤ | 235 (25.66%) | 52 (22.13%) | 64 (27.23%) | 96 (40.85%) | 23 (9.79%) | ||
| History of Childbirth Classes | No | 514 (54.00%) | 105 (20.43%) | 126 (24.51%) | 184 (35.80%) | 99 (19.26%) | 0.014 |
| Yes | 439 (46.00%) | 88 (20.05%) | 95 (21.64%) | 197 (44.87%) | 59 (13.44%) | ||
Table 2 presents components of tokophobia and examines their variation based on childbirth history and method, with statistically significant values reported. Physical summation shows a marked difference between natural and cesarean births (<0.001), indicating that women undergoing cesareans experience higher physical impacts related to tokophobia. Feelings of panic and social involvement also significantly differ (P = 0.0042 and P=0.0041, respectively), with cesarean births correlating with elevated levels of panic and social disruption. Interference with daily habits (<0.001) is notably higher among cesarean cases, indicating that the childbirth method has a significant impact on daily functioning.
Self-perception of tokophobia (<0.001) and the overall tokophobia total score (<0.001) reveal that cesarean births are associated with more pronounced tokophobia compared to natural births. However, avoidance of pregnancy shows no statistically significant difference (P=0.1162), suggesting that this specific component is less influenced by childbirth history or the method of delivery. The findings collectively underscore the heightened psychological and social impacts of tokophobia in cesarean births, emphasizing the need for targeted interventions to manage these experiences.
Self-perception of tokophobia (<0.001) and the overall tokophobia total score (<0.001) reveal that cesarean births are associated with more pronounced tokophobia compared to natural births. However, avoidance of pregnancy shows no statistically significant difference (P=0.1162), suggesting that this specific component is less influenced by childbirth history or the method of delivery. The findings collectively underscore the heightened psychological and social impacts of tokophobia in cesarean births, emphasizing the need for targeted interventions to manage these experiences.
| Tokophobia Component | Do you have a history of childbirth? | P-value | |||
| Yes | No | ||||
| Natural | Cesarean | Probability Natural | Probability Cesarean |
||
| Physical Summation | 12.64 ± 4.80 | 12.31 ± 5.49 | 11.26 ± 4.07 | 13.75 ± 5.24 | < 0.001 |
| Feeling of Panic | 6.52 ± 2.99 | 6.78 ± 3.29 | 6.68 ± 3.03 | 7.65 ± 3.62 | 0.0042 |
| Social Involvement | 6.48 ± 2.80 | 6.57 ± 3.09 | 6.31 ± 2.54 | 7.27 ± 3.13 | 0.0041 |
| Interference with Daily Habits | 7.33 ± 3.10 | 7.37 ± 3.29 | 6.83 ± 2.92 | 8.22 ± 3.39 | < 0.001 |
| Avoidance of Pregnancy | 7.69 ± 3.41 | 7.78 ± 3.61 | 7.29 ± 3.21 | 7.97 ± 3.61 | 0.1162 |
| Self-perception of Tokophobia | 3.66 ± 1.75 | 3.74 ± 1.63 | 3.63 ± 1.65 | 4.41 ± 1.77 | < 0.001 |
| Tokophobia Total | 44.86 ± 15.58 | 44.76 ± 17.09 | 42.01 ± 12.82 | 49.56 ± 15.75 | < 0.001 |
There was a non-significant reduction in tokophobia scores for women with a prior history of childbirth compared to those with a natural birth, attending to the cesarean delivery (β=-0.10, 95% CI:-3.06 to 2.88). Interestingly, women who had no history of childbirth and had a natural delivery showed significantly greater reduction in tokophobia scores (β =-2.85, 95% CI:-5.51 to -0.20). However, this effect lost significance after adjustment (β =-2.18, 95% CI:-4.91 to 0.55). On the other hand, women who did not have any previous childbirth experience and had a cesarean delivery showed significantly higher tokophobia scores in the crude model (β =4.69, 95% CI:1.49 to 7.90), although this association also became non-significant after adjustment (β =3.13, 95% CI:-0.34 to 6.61). These results suggest that certain combinations of childbirth history and delivery method have an impact on variations in tokophobia scores; however, many of these relationships are likely confounded, as most of the effects did not persist after adjustment (Table 3).
Table 3. Linear regression analysis of Tokophobia components based on childbirth history and delivery method
| Crude β (95%CI) |
Crude β (95%CI) |
|
| History of Childbirth/Natural Method of Delivery | 1 | 1 |
| History of Childbirth/Cesarian Method of Delivery | -0.10(-3.06_ 2.88) | -1.58(-4.91_1.73) |
| No History of Childbirth/Natural Method of Delivery | -2.85(-5.51_-0.20) | -2.18(-4.91_0.55) |
| No History of Childbirth/Cesarian Method of Delivery | 4.69(1.49_7.90) | 3.13(-0.34_6.61) |
It can be observed from Figure 1 that the tokophobia scores tend to decrease with the addition of children for both delivery methods, indicating a moderating effect of parity. However, it is noteworthy that women with cesarean deliveries report, by far, higher tokophobia scores in comparison to women who have had natural births, without considering the level of parity. This difference is more pronounced among women with low parity, but does not persist as they have more children. The confidence intervals depicting the confidence level ranges indicate that the perceived discrepancies become more pronounced as the number of children increases, which emphasizes the enduring impact of the method of delivery on tokophobia (Figure 1).
Figure 1. Comparison of Tokophobia scores across childbirth history and delivery methods
Discussion
Our findings indicate that younger women (≤20 years) and those without childbirth experience are more likely to prefer cesarean delivery, possibly due to fear and lack of awareness. In contrast, women with three or more children predominantly opt for natural birth, emphasizing the role of prior experience in delivery decisions. This finding aligns with previous studies [9, 10], although Kosan et al. found no significant association between age and delivery preference [7]. These results highlight the need to educate first-time mothers about childbirth options and the benefits of vaginal delivery.
Housewives showed a higher tendency toward cesarean delivery, consistent with findings from Ghana [9], where employed women were less likely to undergo cesarean sections. However, Nabawanuka et al. reported the opposite in Uganda [11], and other studies found no significant link between employment status and delivery choice [7]. These mixed results suggest that occupational and cultural factors may influence delivery preferences.
Although economic status was not statistically significant in our study, women with better financial conditions had higher rates of cesarean sections. This finding is supported by Tilahun et al. [9], while Kosan et al. found no such association [7]. Access to medical services may explain this trend, underscoring the importance of equitable prenatal care regardless of socioeconomic status.
Women with a history of miscarriage in our sample leaned toward natural birth, contrasting with studies that associate miscarriage history with cesarean preference [12, 13]. These differences may reflect cultural norms, psychological responses, and variations in prenatal counseling. Delivery decisions for these women should be individualized and supported by clinical and emotional care.
Educational level also influenced delivery preference. Women with primary and secondary education were more inclined toward cesarean delivery, while those with higher education and childbirth class attendance favored natural birth. This finding supports previous findings [7, 9, 14] and highlights the role of awareness in reducing unnecessary cesarean sections.
Late-stage pregnancy (≥30 weeks) was associated with increased cesarean preference, likely due to heightened anxiety. This aligns with prior research [15], which emphasizes the need for psychological support and education during the final weeks of pregnancy.
Finally, our results confirm that cesarean delivery is associated with higher levels of tokophobia, including panic, social withdrawal, and disruption of daily life, while pregnancy avoidance remained statistically unchanged [1, 2, 4]. Tokophobia was more pronounced among low-parity women and decreased with childbirth experience. These findings underscore the psychological burden of tokophobia and the need for targeted interventions, including counseling, education, and integration of tokophobia screening into prenatal care. Further research should investigate the long-term psychological effects and effective strategies to mitigate fear and enhance maternal well-being.
This study is strengthened by its large sample size and the inclusion of participants from varied socio-demographic backgrounds, which enhances the external validity and generalizability of the findings. The use of the validated TAQ further contributes to the reliability of psychological measurements. Nonetheless, the reliance on self-reported data may introduce response bias, and the cross-sectional design restricts the ability to draw causal inferences. Additionally, cultural and healthcare system differences may influence participants’ perceptions and responses, warranting cautious interpretation of the results. Despite these limitations, the study offers meaningful insights into childbirth preferences and the psychological dimensions of tokophobia, underscoring the need for targeted educational and clinical interventions. Future research should consider longitudinal approaches to explore the long-term trajectory of tokophobia and develop tailored strategies to reduce childbirth-related fear and support informed maternal decision-making.
Conclusion
Our findings highlight various factors influencing women's childbirth preferences, including age, education, employment status, economic conditions, miscarriage history, and late pregnancy anxiety. Younger and less-educated women tend to prefer cesarean delivery, often due to fear and lack of information, while higher-educated women and those with childbirth experience opt for natural birth. Psychological and social influences play a crucial role, especially in the final weeks of pregnancy. Reducing cesarean rates requires targeted education, psychological counseling, and equitable healthcare policies to support informed decision-making, mitigate anxiety, and promote maternal well-being. Future research should explore long-term psychological effects and effective interventions for tokophobia.
Ethical Considerations
The research ethics committee at Kermanshah University of Medical Sciences, Iran, approved the study protocol (KUMS.REC.1402.590). All procedures adhered to the ethical standards of the institution and the national research committee, as well as the 1964 Helsinki Declaration and its subsequent amendments. Before participating, participants were provided with detailed information about the study, including its procedures, the confidentiality of their information, and its purpose. Informed consent for participation in the study was obtained from all participants. The participants were given the participant information statement and signed the consent form.
Acknowledgments
We extend our heartfelt gratitude to the pregnant women who participated in this study. We also wish to express our appreciation to the Research Vice-Chancellor at Kermanshah University of Medical Sciences, Iran, for their invaluable support in this project.
Authors' Contributions
M.M.A. and F.J. contributed to the interpretation of the study's findings. M.M.N. was involved in data analysis, while N.K. was responsible for drafting the initial version of the manuscript. All authors participated in the final approval of the revised manuscript for publication.
Funding/Support
This study was funded by the Kermanshah University of Medical Sciences, Iran. The funding organizations had no involvement in the study's design, data collection, analysis, interpretation, or manuscript preparation (Project Number: 4020975).
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
Our findings indicate that younger women (≤20 years) and those without childbirth experience are more likely to prefer cesarean delivery, possibly due to fear and lack of awareness. In contrast, women with three or more children predominantly opt for natural birth, emphasizing the role of prior experience in delivery decisions. This finding aligns with previous studies [9, 10], although Kosan et al. found no significant association between age and delivery preference [7]. These results highlight the need to educate first-time mothers about childbirth options and the benefits of vaginal delivery.
Housewives showed a higher tendency toward cesarean delivery, consistent with findings from Ghana [9], where employed women were less likely to undergo cesarean sections. However, Nabawanuka et al. reported the opposite in Uganda [11], and other studies found no significant link between employment status and delivery choice [7]. These mixed results suggest that occupational and cultural factors may influence delivery preferences.
Although economic status was not statistically significant in our study, women with better financial conditions had higher rates of cesarean sections. This finding is supported by Tilahun et al. [9], while Kosan et al. found no such association [7]. Access to medical services may explain this trend, underscoring the importance of equitable prenatal care regardless of socioeconomic status.
Women with a history of miscarriage in our sample leaned toward natural birth, contrasting with studies that associate miscarriage history with cesarean preference [12, 13]. These differences may reflect cultural norms, psychological responses, and variations in prenatal counseling. Delivery decisions for these women should be individualized and supported by clinical and emotional care.
Educational level also influenced delivery preference. Women with primary and secondary education were more inclined toward cesarean delivery, while those with higher education and childbirth class attendance favored natural birth. This finding supports previous findings [7, 9, 14] and highlights the role of awareness in reducing unnecessary cesarean sections.
Late-stage pregnancy (≥30 weeks) was associated with increased cesarean preference, likely due to heightened anxiety. This aligns with prior research [15], which emphasizes the need for psychological support and education during the final weeks of pregnancy.
Finally, our results confirm that cesarean delivery is associated with higher levels of tokophobia, including panic, social withdrawal, and disruption of daily life, while pregnancy avoidance remained statistically unchanged [1, 2, 4]. Tokophobia was more pronounced among low-parity women and decreased with childbirth experience. These findings underscore the psychological burden of tokophobia and the need for targeted interventions, including counseling, education, and integration of tokophobia screening into prenatal care. Further research should investigate the long-term psychological effects and effective strategies to mitigate fear and enhance maternal well-being.
This study is strengthened by its large sample size and the inclusion of participants from varied socio-demographic backgrounds, which enhances the external validity and generalizability of the findings. The use of the validated TAQ further contributes to the reliability of psychological measurements. Nonetheless, the reliance on self-reported data may introduce response bias, and the cross-sectional design restricts the ability to draw causal inferences. Additionally, cultural and healthcare system differences may influence participants’ perceptions and responses, warranting cautious interpretation of the results. Despite these limitations, the study offers meaningful insights into childbirth preferences and the psychological dimensions of tokophobia, underscoring the need for targeted educational and clinical interventions. Future research should consider longitudinal approaches to explore the long-term trajectory of tokophobia and develop tailored strategies to reduce childbirth-related fear and support informed maternal decision-making.
Conclusion
Our findings highlight various factors influencing women's childbirth preferences, including age, education, employment status, economic conditions, miscarriage history, and late pregnancy anxiety. Younger and less-educated women tend to prefer cesarean delivery, often due to fear and lack of information, while higher-educated women and those with childbirth experience opt for natural birth. Psychological and social influences play a crucial role, especially in the final weeks of pregnancy. Reducing cesarean rates requires targeted education, psychological counseling, and equitable healthcare policies to support informed decision-making, mitigate anxiety, and promote maternal well-being. Future research should explore long-term psychological effects and effective interventions for tokophobia.
Ethical Considerations
The research ethics committee at Kermanshah University of Medical Sciences, Iran, approved the study protocol (KUMS.REC.1402.590). All procedures adhered to the ethical standards of the institution and the national research committee, as well as the 1964 Helsinki Declaration and its subsequent amendments. Before participating, participants were provided with detailed information about the study, including its procedures, the confidentiality of their information, and its purpose. Informed consent for participation in the study was obtained from all participants. The participants were given the participant information statement and signed the consent form.
Acknowledgments
We extend our heartfelt gratitude to the pregnant women who participated in this study. We also wish to express our appreciation to the Research Vice-Chancellor at Kermanshah University of Medical Sciences, Iran, for their invaluable support in this project.
Authors' Contributions
M.M.A. and F.J. contributed to the interpretation of the study's findings. M.M.N. was involved in data analysis, while N.K. was responsible for drafting the initial version of the manuscript. All authors participated in the final approval of the revised manuscript for publication.
Funding/Support
This study was funded by the Kermanshah University of Medical Sciences, Iran. The funding organizations had no involvement in the study's design, data collection, analysis, interpretation, or manuscript preparation (Project Number: 4020975).
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- Abdelaziz EM, Alshammari AM, Elsharkawy NB, Oraby FA, Ramadan OM. Digital intervention for tokophobia: a randomized controlled trial of internet-based cognitive behavioral therapy on fear of childbirth and self-efficacy among Egyptian pregnant women. BMC Pregnancy Childbirth. 2025;25(1):233. [DOI: 10.1186/s12884-025-07341-5] [PMID] [PMCID]
- Çubukçu B, Şahin SA. The effect of pregnant women's childbirth beliefs on fear of childbirth. Women's Studies Int Forum. 2025;108:103017. [DOI:10.1016/j.wsif.2024.103017]
- Ortega-Cejas CM, Roldán-Merino J, Lluch-Canut T, Castrillo-Pérez MI, Vicente-Hernández MM, Jimenez-Barragan M, et al. Reliability and validity study of the Spanish adaptation of the “Wijma delivery expectancy/experience questionnaire”(W-DEQ-A). Plos One. 2021;16(3):e0248595. [DOI: 10.1371/journal.pone.0248595] [PMID] [PMCID]
- Kalok A, Kamisan Atan I, Sharip S, Safian N, Shah SA. Factors influencing childbirth fear among Asian women: a scoping review. Front Public Health. 2025;12:1448940. [DOI: 10.3389/fpubh.2024.1448940] [PMID] [PMCID]
- Çapik A, Durmaz H. Fear of childbirth, postpartum depression, and birth‐related variables as predictors of posttraumatic stress disorder after childbirth. Worldviews Evid Based Nurs. 2018;15(6):455-63. [DOI: 10.1111/wvn.12326] [PMID]
- Dal Moro AP, Soecki G, de Fraga FS, Petterle RR, Rückl SZ. Fear of childbirth: prevalence and associated factors in pregnant women of a maternity hospital in southern Brazil. BMC Pregnancy Childbirth. 2023;23(1):632. [DOI: 10.1186/s12884-023-05948-0] [PMID] [PMCID]
- Kosan Z, Kavuncuoglu D, Calıkoglu EO, Aras A. Delivery preferences of pregnant women: Do not underestimate the effect of friends and relatives. J Gynecol Obstet Hum Reprod. 2019;48(6):395-400. [DOI: 10.1016/j.jogoh.2019.03.009]
- Nunes RD, Traebert E, Seemann M, Traebert J. Tokophobia Assessment Questionnaire: a new instrument. Braz J Psychiatry. 2020;43(1):112-114. [DOI: 10.1590/1516-4446-2020-1252] [PMID]
- Tilahun WM, Simegn MB, Abate A, Golla EB, Ali MA, Kumbi H, et al. Caesarean section delivery and its associated factors in Ghana: A multilevel analysis. PloS one. 2025; 20(2):e0318223. [DOI: 10.1371/journal.pone.0318223] [PMID]
- Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PloS One. 2016;11(2):e0148343. [DOI: 10.1371/journal.pone.0148343] [PMID] [PMCID]
- Nabawanuka B, Ngabirano T, Nankumbi J. Preference and determinants of delivery mode in pregnant women with one cesarean scar: a cross-sectional study in two urban Ugandan public hospitals. BMC Pregnancy Childbirth. 2025;25(1):127. [DOI: 10.1186/s12884-025-07263-2] [PMID] [PMCID]
- Ye L, Cao W, Yao J, Peng G, Zhou R. Systematic review of the effects of birth spacing after cesarean delivery on maternal and perinatal outcomes. Int J Gynecol Obstet. 2019;147(1):19-28. [DOI: 10.1002/ijgo.12895] [PMID]
- Taye BA, Weldearegay BY, Yirsaw BG, Demsie ME, Asfaw FF, Teka AB, et al. Preference of mode of delivery and associated factors among mothers in East Africa: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2025; 25(1):232. [DOI: 10.1186/s12884-025-07287-8] [PMID]
- Wax JR, CartinA, Pinette MG, Blackstone J. Patient choice cesarean—the Maine experience. Birth. 2005;32(3):203-206. [DOI: 10.1111/j.0730-7659.2005.00370.x] [PMID]
- Naylor Smith J, Taylor B, Shaw K, Hewison A, Kenyon S. ‘I didn’t think you were allowed that, they didn’t mention that.’A qualitative study exploring women’s perceptions of home birth. BMC pregnancy childbirth. 2018;18(1):105. [DOI: 10.1186/s12884-018-1733-1] [PMID] [PMCID]
Article Type: Research Article |
Subject:
Mother and child health
Received: 2025/05/20 | Accepted: 2025/06/15 | Published: 2025/06/20
Received: 2025/05/20 | Accepted: 2025/06/15 | Published: 2025/06/20
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |