Volume 12, Issue 1 (February 2025)
Avicenna J Neuro Psycho Physiology 2025, 12(1): 17-25 |
Back to browse issues page
Ethics code: IR.ACECR.ROYAN.REC.1401.063
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sadeghian Motahar S M, Fata L, Keshmiri M, Kachooei M. A Grounded Theory Analysis of Disgust Mechanisms in Patients with Contamination-related Obsessive-compulsive Disorder: A Mixed-Methods Investigation. Avicenna J Neuro Psycho Physiology 2025; 12 (1) :17-25
URL: http://ajnpp.umsha.ac.ir/article-1-519-en.html
URL: http://ajnpp.umsha.ac.ir/article-1-519-en.html
1- Ph.D. Candidate in Psychology, Department of Psychology, Faculty of Humanities, University of Science and Culture, Tehran, Iran.
2- Ph.D. in Psychology, Department of Psychology, Faculty of Humanities, Iran University of Medical Science, Tehran, Iran ,ladanfata@gmail.com
3- Ph.D. in Psychology, Assistant Professor, Department of Psychology, Faculty of Humanities, University of Science and Culture, Tehran, Iran
4- Ph.D. in Psychology, Department of Psychology, Faculty of Humanities, University of Science and Culture, Tehran, Iran
2- Ph.D. in Psychology, Department of Psychology, Faculty of Humanities, Iran University of Medical Science, Tehran, Iran ,
3- Ph.D. in Psychology, Assistant Professor, Department of Psychology, Faculty of Humanities, University of Science and Culture, Tehran, Iran
4- Ph.D. in Psychology, Department of Psychology, Faculty of Humanities, University of Science and Culture, Tehran, Iran
Keywords: Obsessive-compulsive disorder, Disgust, Compulsive behavior, Qualitative research, Structural equation modeling, Mixed methods
Full-Text [PDF 465 kb]
(230 Downloads)
| Abstract (HTML) (1420 Views)
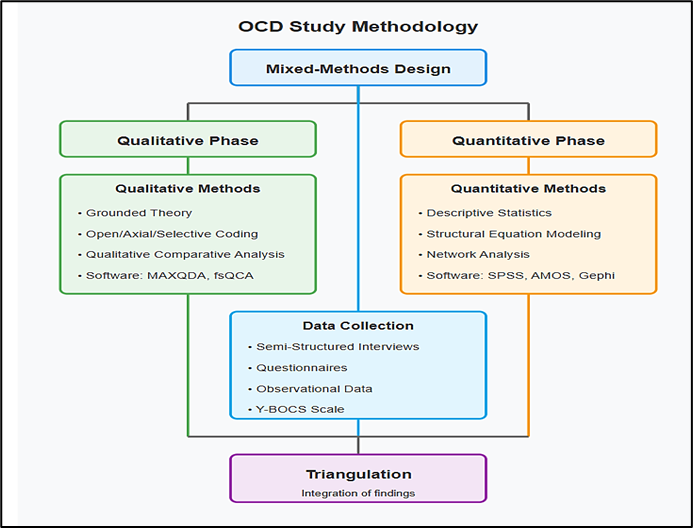
Figure 1. Methodological framework for contamination-based obsessive-compulsive disorder research study
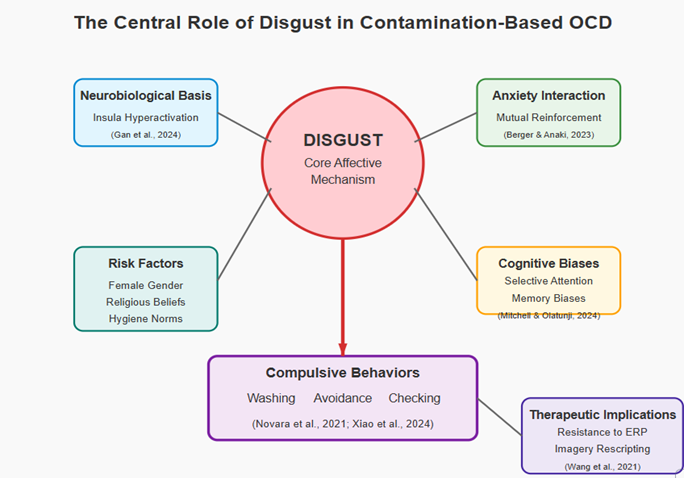
Figure 2. An integrated model of disgust as a core mechanism in contamination-based obsessive-compulsive disorder
References
Full-Text: (256 Views)
Background
Obsessive–Compulsive Disorder (OCD) is a complex and chronic psychological condition characterized by intrusive, unwanted thoughts (obsessions) and repetitive, compulsive behaviors (compulsions). Among its clinical subtypes, contamination-based OCD is one of the most common and severe forms. Individuals with this subtype often experience an overwhelming fear of physical, chemical, or even moral and mental contamination, which leads to ritualistic behaviors, such as excessive washing, avoidance of particular objects or environments, and compulsive cleansing of the body or mind [1]. Historically, dominant theories have framed anxiety as the central emotion underlying OCD, and treatment approaches—particularly Exposure and Response Prevention—have been developed accordingly. However, an increasing body of contemporary research suggests that disgust–especially in the contamination subtype–plays a more critical role than anxiety. Disgust is a basic emotion with evolutionary roots that serves to protect the body from potential sources of disease and decay. However, this emotion is experienced with unusual intensity and breadth in individuals with contamination-based OCD [2].
Empirical findings, including neuroimaging studies (e.g., functional magnetic resonance imaging), have shown that specific brain regions, such as the insula, which is involved in disgust processing, display hyperactivity in individuals with this subtype of OCD. In addition, psychometric and behavioral studies have demonstrated that these individuals exhibit significantly higher levels of disgust sensitivity, which directly predicts avoidant behaviors, compulsive washing, and functional impairment in social and occupational settings [3].
The evolving understanding of OCD—from early psychodynamic views to modern cognitive-behavioral and neurobiological models—has led to its reclassification in the DSM-5 under a distinct category: Obsessive–Compulsive and Related Disorders. Recent studies have highlighted the role of not only serotonergic systems but also glutamatergic neurotransmission and genetic variations linked to OCD vulnerability [4, 5]. Genetic studies have shown elevated heritability, particularly in monozygotic twins [6], while environmental factors, such as trauma and early adverse experiences, also contribute to the onset and exacerbation of this disorder [7].
Among all OCD subtypes, contamination OCD has been identified as the most prevalent and functionally impairing. It involves two main forms: contact contamination, which relates to direct exposure to perceived dirty or toxic materials; and mental contamination, characterized by an internal sense of impurity often rooted in guilt, shame, or moral violation [8]. Research has shown that both subtypes are closely linked to intensified disgust reactivity and evading tendencies [9].
Neuroscientific research has consistently demonstrated that disgust-related stimuli elicit stronger activation in brain regions, such as the insula and amygdala, in individuals with OCD, compared to healthy controls [10, 11]. Cognitive theories further emphasize the role of disgust-related biases in memory and attention, whereby individuals are more likely to recall and attend to contamination-related stimuli [12]. Cultural and religious contexts further shape the expression and intensity of symptoms, with higher prevalence and severity reported in societies that emphasize hygiene, morality, and ritual purity [13, 14].
Recent global events, such as the COVID-19 pandemic, have also highlighted the amplification of contamination fears and disgust-driven behaviors among OCD patients [15]. This has drawn renewed attention to the functional role of disgust as a motivator for avoidance and safety behaviors, especially during periods of public health crises [16].
Despite this growing body of literature, the current theoretical and empirical research presents two critical limitations. First, most studies rely on quantitative methodologies and closed-ended instruments that fail to capture the depth and complexity of lived experience. Second, existing models provide only a fragmented understanding of the causal and contextual mechanisms through which disgust contributes to the onset, maintenance, and variation of compulsive behaviors across individuals and cultures.
In response to this gap, the present study employed a Grounded Theory methodology, using semi-structured interviews with individuals diagnosed with contamination-based OCD. This research aimed to identify the conceptual structures and underlying psychosocial mechanisms that govern the experience of disgust and to construct a multilayered model that elucidates how this emotion contributes to the trajectory of compulsive behaviors. By focusing on the lived experiences of participants and interpreting them through phenomenological, interpretive, and analytical lenses, this research endeavored to develop a more comprehensive theoretical framework for understanding OCD and to inform more culturally sensitive and emotion-targeted therapeutic interventions.
Objectives
Contamination-based OCD is a prevalent and functionally impairing subtype among clinical populations. However, there is limited empirical research exploring the multidimensional role of disgust in the onset and maintenance of this condition. This study aimed to examine the cognitive, emotional, and sociocultural mechanisms underlying disgust in individuals with contamination-based OCD, using a mixed-methods approach that included Grounded Theory, Structural Equation Modeling (SEM), network analysis, and fuzzy-set Qualitative Comparative Analysis (fsQCA), to inform the development of more targeted and culturally sensitive interventions.
Materials and Methods
This study employed a convergent mixed-methods design, integrating qualitative and quantitative approaches to investigate the role of disgust in contamination-based OCD. The qualitative phase was based on Grounded Theory methodology (Strauss and Corbin) to explore the formation and structure of disgust-related responses. The quantitative phase included descriptive and inferential statistics, SEM, and network analysis to examine associations between variables.
The study was theoretically grounded in cognitive-behavioral models of OCD and contemporary theories of disgust, which informed the development of interview protocols, instruments, and coding frameworks. The integration of these models supported both the design and interpretation of qualitative and quantitative findings.
In total, 30 adult participants, aged between 22 and 42 years, were recruited from clinical settings. All participants had a formal diagnosis of contamination-based OCD, confirmed according to DSM-5 or ICD-10 criteria by a licensed clinical psychiatrist. Eligibility criteria required the presence of at least one compulsive behavior, such as washing, checking, or avoidance, as well as elevated disgust sensitivity.
Inclusion criteria were as follows: a clinically confirmed diagnosis of contamination-based OCD, evidence of compulsive behaviors and high disgust sensitivity, age between 20 and 45 years, proficiency in verbal and written communication, and signed informed consent. Exclusion criteria consisted of the following: more than 20% missing data, voluntary withdrawal, severe psychiatric or neurological comorbidities, inability to provide reliable self-report, or life events that interfered with participation.
Data collection instruments included the following:
Semi-Structured Interviews: Custom-developed interviews, informed by cognitive-behavioral and emotion theories, were used to assess emotional responses of participants, behavioral patterns, and sociocultural influences. Each interview session lasted between 45 and 60 min, was audio-recorded with the consent of the participant, and subsequently transcribed verbatim for analysis.
Standardized Questionnaires: These included the Disgust Sensitivity Scale (5-point Likert scale; Cronbach’s alpha = 0.84), the Obsessive–Compulsive Behavior Checklist, a demographic data form (capturing age, gender, education, marital status, and income), and the Yale Brown Obsessive Compulsive Scale for assessing symptom severity [17].
Behavioral Observations: Naturalistic observations were conducted either in the home or workplace settings of participants. These observations were documented using detailed field notes and standardized checklists. Key behaviors assessed included washing, checking, and avoidance [17].
Statistical analyses were conducted using SPSS version 15.0 (IBM Corp., Armonk, NY, USA) to perform both descriptive statistics including mean, standard deviation, and frequency and inferential tests such as t-tests, ANOVA, and logistic regression. AMOS version 24 (IBM Corp.) was employed for structural equation modeling (SEM) and path modeling. Additionally, network structures and heatmaps were visualized using Gephi software version 0.10 (Gephi Consortium, WebAtlas, Paris, France). Post hoc Tukey tests were used to examine between-group differences, and multilevel modeling was applied to assess both individual and group-level effects.
For qualitative data analysis, MAXQDA version 20 (VERBI GmbH, Berlin, Germany) was utilized to code and analyze interview transcripts using open, axial, and selective coding strategies. Fuzzy-set Qualitative Comparative Analysis (fsQCA) and Q-methodology were employed to identify specific cognitive-behavioral configurations and subjective belief patterns related to disgust. As part of the Q-analysis, participants sorted belief statements regarding disgust, and these responses were analyzed using PQMethod version 2.35 (available at qmethod.org). This analysis revealed three core factors: sensitivity to contamination, safety-oriented cognition, and a preference for order and control. Triangulation was used to integrate findings across qualitative and quantitative methods, thereby enhancing the interpretive robustness of the study. Furthermore, graphical outputs and factor maps were generated to visualize both convergent and divergent themes, following the methodology outlined by Gonçalves et al. [18].
To ensure the reliability and validity of the findings, several methodological safeguards were implemented. Internal consistency was assessed using Cronbach’s alpha, while inter-rater reliability was measured with Cohen’s kappa (κ = 0.78), which evaluated coding agreement among the researchers. The credibility and authenticity of the qualitative findings were further supported by member checking and peer debriefing processes [19]. Q-analysis was carried out to further examine cognitive patterns of participants concerning disgust and obsessive-compulsive disorder. Participants were asked to rank belief statements, which were then analyzed with PQMethod software. This process helped to identify three dominant themes: sensitivity to contamination, concern for safety, and a strong preference for order and control.
This study relied on several software tools for both data analysis and integration. Quantitative statistical analysis was conducted in SPSS, while SEM was performed in AMOS, and Network analysis was carried out in Gephi software. For qualitative and Q-analysis, MAXQDA, fsQCA, and PQMethod software were used. Furthermore, data visualization and triangulation tools were employed to enhance clarity and conceptual integration.
Specifically, SPSS software was used for quantitative analysis, AMOS for SEM, Gephi for network analysis, MAXQDA for qualitative coding, fsQCA (version 3.0) for causal configuration analysis, and PQMethod for Q-methodology, as described by Ali et al. [20].
The mixed-methods approach used for studying disgust and compulsive behaviors in contamination-based OCD integrated qualitative methodologies, such as grounded theory and systematic coding techniques, with quantitative approaches, including statistical analysis, SEM, and network modeling. Data were collected through interviews, standardized questionnaires, behavioral observations, and clinical scales. The study concluded with triangulation to merge findings from both methodological strands, providing a comprehensive and nuanced understanding of the phenomenon.
Empirical findings, including neuroimaging studies (e.g., functional magnetic resonance imaging), have shown that specific brain regions, such as the insula, which is involved in disgust processing, display hyperactivity in individuals with this subtype of OCD. In addition, psychometric and behavioral studies have demonstrated that these individuals exhibit significantly higher levels of disgust sensitivity, which directly predicts avoidant behaviors, compulsive washing, and functional impairment in social and occupational settings [3].
The evolving understanding of OCD—from early psychodynamic views to modern cognitive-behavioral and neurobiological models—has led to its reclassification in the DSM-5 under a distinct category: Obsessive–Compulsive and Related Disorders. Recent studies have highlighted the role of not only serotonergic systems but also glutamatergic neurotransmission and genetic variations linked to OCD vulnerability [4, 5]. Genetic studies have shown elevated heritability, particularly in monozygotic twins [6], while environmental factors, such as trauma and early adverse experiences, also contribute to the onset and exacerbation of this disorder [7].
Among all OCD subtypes, contamination OCD has been identified as the most prevalent and functionally impairing. It involves two main forms: contact contamination, which relates to direct exposure to perceived dirty or toxic materials; and mental contamination, characterized by an internal sense of impurity often rooted in guilt, shame, or moral violation [8]. Research has shown that both subtypes are closely linked to intensified disgust reactivity and evading tendencies [9].
Neuroscientific research has consistently demonstrated that disgust-related stimuli elicit stronger activation in brain regions, such as the insula and amygdala, in individuals with OCD, compared to healthy controls [10, 11]. Cognitive theories further emphasize the role of disgust-related biases in memory and attention, whereby individuals are more likely to recall and attend to contamination-related stimuli [12]. Cultural and religious contexts further shape the expression and intensity of symptoms, with higher prevalence and severity reported in societies that emphasize hygiene, morality, and ritual purity [13, 14].
Recent global events, such as the COVID-19 pandemic, have also highlighted the amplification of contamination fears and disgust-driven behaviors among OCD patients [15]. This has drawn renewed attention to the functional role of disgust as a motivator for avoidance and safety behaviors, especially during periods of public health crises [16].
Despite this growing body of literature, the current theoretical and empirical research presents two critical limitations. First, most studies rely on quantitative methodologies and closed-ended instruments that fail to capture the depth and complexity of lived experience. Second, existing models provide only a fragmented understanding of the causal and contextual mechanisms through which disgust contributes to the onset, maintenance, and variation of compulsive behaviors across individuals and cultures.
In response to this gap, the present study employed a Grounded Theory methodology, using semi-structured interviews with individuals diagnosed with contamination-based OCD. This research aimed to identify the conceptual structures and underlying psychosocial mechanisms that govern the experience of disgust and to construct a multilayered model that elucidates how this emotion contributes to the trajectory of compulsive behaviors. By focusing on the lived experiences of participants and interpreting them through phenomenological, interpretive, and analytical lenses, this research endeavored to develop a more comprehensive theoretical framework for understanding OCD and to inform more culturally sensitive and emotion-targeted therapeutic interventions.
Objectives
Contamination-based OCD is a prevalent and functionally impairing subtype among clinical populations. However, there is limited empirical research exploring the multidimensional role of disgust in the onset and maintenance of this condition. This study aimed to examine the cognitive, emotional, and sociocultural mechanisms underlying disgust in individuals with contamination-based OCD, using a mixed-methods approach that included Grounded Theory, Structural Equation Modeling (SEM), network analysis, and fuzzy-set Qualitative Comparative Analysis (fsQCA), to inform the development of more targeted and culturally sensitive interventions.
Materials and Methods
This study employed a convergent mixed-methods design, integrating qualitative and quantitative approaches to investigate the role of disgust in contamination-based OCD. The qualitative phase was based on Grounded Theory methodology (Strauss and Corbin) to explore the formation and structure of disgust-related responses. The quantitative phase included descriptive and inferential statistics, SEM, and network analysis to examine associations between variables.
The study was theoretically grounded in cognitive-behavioral models of OCD and contemporary theories of disgust, which informed the development of interview protocols, instruments, and coding frameworks. The integration of these models supported both the design and interpretation of qualitative and quantitative findings.
In total, 30 adult participants, aged between 22 and 42 years, were recruited from clinical settings. All participants had a formal diagnosis of contamination-based OCD, confirmed according to DSM-5 or ICD-10 criteria by a licensed clinical psychiatrist. Eligibility criteria required the presence of at least one compulsive behavior, such as washing, checking, or avoidance, as well as elevated disgust sensitivity.
Inclusion criteria were as follows: a clinically confirmed diagnosis of contamination-based OCD, evidence of compulsive behaviors and high disgust sensitivity, age between 20 and 45 years, proficiency in verbal and written communication, and signed informed consent. Exclusion criteria consisted of the following: more than 20% missing data, voluntary withdrawal, severe psychiatric or neurological comorbidities, inability to provide reliable self-report, or life events that interfered with participation.
Data collection instruments included the following:
Semi-Structured Interviews: Custom-developed interviews, informed by cognitive-behavioral and emotion theories, were used to assess emotional responses of participants, behavioral patterns, and sociocultural influences. Each interview session lasted between 45 and 60 min, was audio-recorded with the consent of the participant, and subsequently transcribed verbatim for analysis.
Standardized Questionnaires: These included the Disgust Sensitivity Scale (5-point Likert scale; Cronbach’s alpha = 0.84), the Obsessive–Compulsive Behavior Checklist, a demographic data form (capturing age, gender, education, marital status, and income), and the Yale Brown Obsessive Compulsive Scale for assessing symptom severity [17].
Behavioral Observations: Naturalistic observations were conducted either in the home or workplace settings of participants. These observations were documented using detailed field notes and standardized checklists. Key behaviors assessed included washing, checking, and avoidance [17].
Statistical analyses were conducted using SPSS version 15.0 (IBM Corp., Armonk, NY, USA) to perform both descriptive statistics including mean, standard deviation, and frequency and inferential tests such as t-tests, ANOVA, and logistic regression. AMOS version 24 (IBM Corp.) was employed for structural equation modeling (SEM) and path modeling. Additionally, network structures and heatmaps were visualized using Gephi software version 0.10 (Gephi Consortium, WebAtlas, Paris, France). Post hoc Tukey tests were used to examine between-group differences, and multilevel modeling was applied to assess both individual and group-level effects.
For qualitative data analysis, MAXQDA version 20 (VERBI GmbH, Berlin, Germany) was utilized to code and analyze interview transcripts using open, axial, and selective coding strategies. Fuzzy-set Qualitative Comparative Analysis (fsQCA) and Q-methodology were employed to identify specific cognitive-behavioral configurations and subjective belief patterns related to disgust. As part of the Q-analysis, participants sorted belief statements regarding disgust, and these responses were analyzed using PQMethod version 2.35 (available at qmethod.org). This analysis revealed three core factors: sensitivity to contamination, safety-oriented cognition, and a preference for order and control. Triangulation was used to integrate findings across qualitative and quantitative methods, thereby enhancing the interpretive robustness of the study. Furthermore, graphical outputs and factor maps were generated to visualize both convergent and divergent themes, following the methodology outlined by Gonçalves et al. [18].
To ensure the reliability and validity of the findings, several methodological safeguards were implemented. Internal consistency was assessed using Cronbach’s alpha, while inter-rater reliability was measured with Cohen’s kappa (κ = 0.78), which evaluated coding agreement among the researchers. The credibility and authenticity of the qualitative findings were further supported by member checking and peer debriefing processes [19]. Q-analysis was carried out to further examine cognitive patterns of participants concerning disgust and obsessive-compulsive disorder. Participants were asked to rank belief statements, which were then analyzed with PQMethod software. This process helped to identify three dominant themes: sensitivity to contamination, concern for safety, and a strong preference for order and control.
This study relied on several software tools for both data analysis and integration. Quantitative statistical analysis was conducted in SPSS, while SEM was performed in AMOS, and Network analysis was carried out in Gephi software. For qualitative and Q-analysis, MAXQDA, fsQCA, and PQMethod software were used. Furthermore, data visualization and triangulation tools were employed to enhance clarity and conceptual integration.
Specifically, SPSS software was used for quantitative analysis, AMOS for SEM, Gephi for network analysis, MAXQDA for qualitative coding, fsQCA (version 3.0) for causal configuration analysis, and PQMethod for Q-methodology, as described by Ali et al. [20].
The mixed-methods approach used for studying disgust and compulsive behaviors in contamination-based OCD integrated qualitative methodologies, such as grounded theory and systematic coding techniques, with quantitative approaches, including statistical analysis, SEM, and network modeling. Data were collected through interviews, standardized questionnaires, behavioral observations, and clinical scales. The study concluded with triangulation to merge findings from both methodological strands, providing a comprehensive and nuanced understanding of the phenomenon.
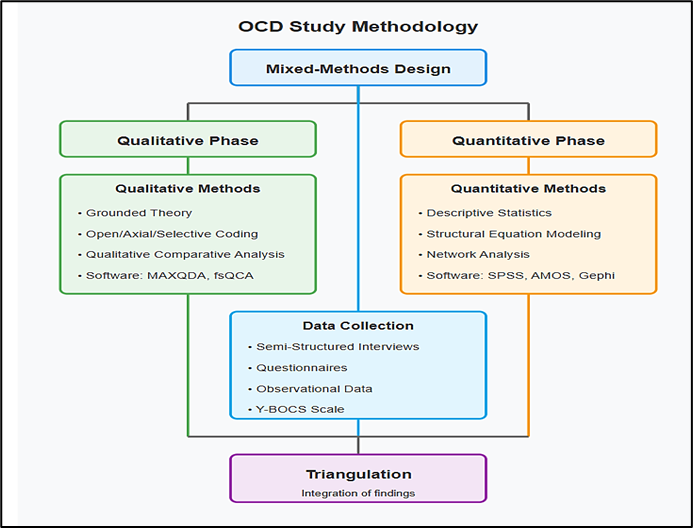
Figure 1. Methodological framework for contamination-based obsessive-compulsive disorder research study
Results
Thirty participants (16 females, 53.3%; 14 males, 46.7%) diagnosed with contamination-based OCD were included in this study. Participants were aged between 22 and 42 years (mean age = 31.8, SD = 5.4). Their educational levels varied, with most participants holding undergraduate (n = 18) or postgraduate degrees (n = 10). Marital status was equally distributed, as 15 participants were unmarried and 15 were married. Income levels ranged from low to high. The demographic data were utilized in subsequent analyses to assess their association with obsessive-compulsive behaviors and disgust sensitivity.
Thematic Analysis (Grounded Theory)
Through open coding of semi-structured interviews and observational data, seven major themes were identified (Table 1).
The core category emerging from selective coding was disgust as a motivational driver of compulsive behaviors. High levels of disgust were consistently associated with washing and avoidance behaviors, while security-related compulsions were primarily linked to anxiety and uncertainty. This distinction informed the integration of emotional and behavioral patterns within the final theoretical model.
Table 1. Identified themes and frequencies
Table 2. Frequency of compulsive behavior types
Table 3. Mean Disgust intensity across themes
Discussion
This study sought to explore the central role of disgust in contamination-based OCD through a mixed-methods approach, integrating qualitative data from semi-structured interviews with quantitative findings from SEM, network analysis, and fsQCA. The results affirmed the hypothesis that disgust is not a peripheral emotion in OCD but functions as a core affective mechanism that significantly drives compulsive behaviors—particularly washing and avoidance—among individuals with this subtype.
Consistent with prior research, a strong association was found between disgust sensitivity and compulsive washing [2, 21]. Disgust intensity was highest among behaviors involving avoidance of contamination and sensitivity to public spaces, supporting previous findings that link disgust to contamination fears and interpersonal avoidance [22]. Neurobiological literature underscores these findings, highlighting the involvement of the insula in disgust processing and its hyperactivation in OCD patients [9, 23].
The SEM and network analysis further revealed that disgust and anxiety interact in reinforcing compulsive behaviors, particularly through feedback loops between emotional reactivity and ritual actions, a concept supported by Berger and Anaki [24]. Cognitive biases, such as selective attention to contamination cues and heightened memory recall of disgusting stimuli, exacerbate the perception of threat [10, 25].
The findings additionally supported the fsQCA model, showing that unmarried women with high disgust sensitivity are most likely to present with washing-related compulsions. These gender differences may be partially attributed to sociocultural norms and role expectations [14, 26]. Religious beliefs, strict childhood hygiene norms, and economic stressors were also identified as contextual modifiers, in line with the law of contagion and culturally reinforced fears [27, 28].
Importantly, this study highlights that disgust demonstrates greater resistance to traditional Exposure and Response Prevention interventions, compared to anxiety, suggesting a need for tailored therapeutic strategies [29]. Emerging modalities, such as imagery rescripting [30] and deep brain stimulation [31], show promise for addressing these limitations.
Despite its strengths, the study had some limitations. First, the sample size was relatively small (N = 30), which may limit the generalizability of quantitative findings. Second, all participants were recruited from clinical settings, possibly skewing responses toward more severe symptomatology. Third, cultural factors were explored in depth but may not be universally generalizable beyond the Iranian context.
Future research should expand to cross-cultural comparisons and longitudinal designs to examine changes in disgust sensitivity over time. The development of disgust-specific therapeutic protocols—potentially integrating cognitive bias modification or targeted neurofeedback—is also recommended. Additional experimental work using neuroimaging could clarify the neural circuits involved in disgust regulation.
Figure 2 presents a conceptual model of how disgust functions as a central driving mechanism in contamination-based OCD. Based on our mixed-methods investigation combining qualitative interviews with advanced quantitative analyses (SEM, network analysis, and fsQCA), the model illustrates the role of disgust not merely as a secondary emotional response but as a fundamental affective component that generates and maintains compulsive behaviors in this OCD subtype.
Thirty participants (16 females, 53.3%; 14 males, 46.7%) diagnosed with contamination-based OCD were included in this study. Participants were aged between 22 and 42 years (mean age = 31.8, SD = 5.4). Their educational levels varied, with most participants holding undergraduate (n = 18) or postgraduate degrees (n = 10). Marital status was equally distributed, as 15 participants were unmarried and 15 were married. Income levels ranged from low to high. The demographic data were utilized in subsequent analyses to assess their association with obsessive-compulsive behaviors and disgust sensitivity.
Thematic Analysis (Grounded Theory)
Through open coding of semi-structured interviews and observational data, seven major themes were identified (Table 1).
The core category emerging from selective coding was disgust as a motivational driver of compulsive behaviors. High levels of disgust were consistently associated with washing and avoidance behaviors, while security-related compulsions were primarily linked to anxiety and uncertainty. This distinction informed the integration of emotional and behavioral patterns within the final theoretical model.
Table 1. Identified themes and frequencies
| Theme | Frequency (n) | Percentage (%) |
| Repetitive washing | 14 | 46.7 |
| Sensitivity to cleanliness | 12 | 40.0 |
| Avoidance of contamination | 11 | 36.7 |
| Sensitivity to public spaces | 6 | 20.0 |
| Security-related compulsions | 5 | 16.7 |
| Belief in insufficient cleaning | 5 | 16.7 |
| Psychological roots | 5 | 16.7 |
Table 2 presents the distribution of compulsive behavior types among participants diagnosed with contamination-based OCD.
The most prevalent behavior was washing and cleanliness rituals, reported by 73.3% of participants. This dominance underscores the central role of contamination fears and disgust sensitivity in driving compulsive handwashing, surface cleaning, and avoidance behaviors. Checking and control behaviors (16.7%) were less frequent and typically associated with security concerns, such as locking doors or turning off appliances. A small subset (3.3%) of participants exhibited order and symmetry behaviors, suggesting that while present, these compulsions were not central to the contamination-based OCD subtype under investigation. These findings align with theoretical frameworks suggesting that disgust predominantly fuels washing-related compulsions in this population.
The most prevalent behavior was washing and cleanliness rituals, reported by 73.3% of participants. This dominance underscores the central role of contamination fears and disgust sensitivity in driving compulsive handwashing, surface cleaning, and avoidance behaviors. Checking and control behaviors (16.7%) were less frequent and typically associated with security concerns, such as locking doors or turning off appliances. A small subset (3.3%) of participants exhibited order and symmetry behaviors, suggesting that while present, these compulsions were not central to the contamination-based OCD subtype under investigation. These findings align with theoretical frameworks suggesting that disgust predominantly fuels washing-related compulsions in this population.
Table 2. Frequency of compulsive behavior types
| Behavior Type | Frequency (n) | Percentage (%) |
| Washing/Cleanliness | 22 | 73.3 |
| Checking/Control | 5 | 16.7 |
| Order/Symmetry | 1 | 3.3 |
Chi-square tests identified a significant gender difference in contamination avoidance behaviors (χ2 = 4.81, p = 0.03), with 9 females versus 2 males reporting these behaviors. However, differences in washing (p = 0.23) and checking behaviors (p = 0.09) were not statistically significant.
Analysis of variance revealed significant differences in disgust intensity across the seven identified themes (F (6, 52) = 5.62, p = 0.001). Results are summarized in Table 3.
Analysis of variance revealed significant differences in disgust intensity across the seven identified themes (F (6, 52) = 5.62, p = 0.001). Results are summarized in Table 3.
Table 3. Mean Disgust intensity across themes
| Theme | Mean | SD |
| Avoidance of contamination | 4.7 | 0.47 |
| Sensitivity to public spaces | 4.8 | 0.41 |
| Repetitive washing | 4.2 | 0.70 |
| Sensitivity to cleanliness | 4.3 | 0.65 |
| Belief in insufficient cleaning | 4.2 | 0.45 |
| Psychological roots | 3.8 | 0.84 |
| Security-related compulsions | 3.2 | 0.45 |
Post hoc Tukey’s test indicated significantly higher disgust levels in avoidance and public space sensitivity, compared to security-related compulsions. The SEM using AMOS revealed a significant path from disgust sensitivity to compulsive washing behavior (β = 0.61, p < 0.001) and from disgust to contamination avoidance (β = 0.58, p < 0.01), supporting the central role of disgust in behavioral activation. Anxiety was found to mediate the relationship between perceived contamination and checking behaviors (β = 0.47, p < 0.05). Model fit indices indicated acceptable fit (CFI = 0.92, RMSEA = 0.06).
Network analysis (conducted in Gephi software) illustrated a densely connected cluster linking disgust-related variables with behavioral outcomes, such as washing and avoidance. Key nodes with high centrality included 'disgust sensitivity', 'contamination avoidance', and 'hand washing'. These findings visually confirmed the interconnected nature of emotional and behavioral dimensions of OCD.
Pearson’s correlation showed a significant positive relationship between disgust intensity and number of obsessive-compulsive behaviors (r = 0.42, p = 0.02). Independent samples t-tests revealed higher disgust in participants exhibiting avoidance behaviors, compared to those with checking behaviors (t(20) = 6.87, p < 0.001). Logistic regression showed that higher disgust scores significantly predicted avoidance behavior (OR = 2.3, 95% CI [1.4, 3.6], p = 0.004).
Reliability and Validity
The internal consistency of the Disgust Sensitivity Scale was high (Cronbach’s α = 0.84), and inter-rater reliability of qualitative coding was acceptable (Cohen’s κ = 0.78). Member checking with selected participants confirmed the accuracy of identified themes. Peer debriefing supported the credibility and confirmability of qualitative results.
Using PQMethod software, three cognitive response patterns were extracted:
Network analysis (conducted in Gephi software) illustrated a densely connected cluster linking disgust-related variables with behavioral outcomes, such as washing and avoidance. Key nodes with high centrality included 'disgust sensitivity', 'contamination avoidance', and 'hand washing'. These findings visually confirmed the interconnected nature of emotional and behavioral dimensions of OCD.
Pearson’s correlation showed a significant positive relationship between disgust intensity and number of obsessive-compulsive behaviors (r = 0.42, p = 0.02). Independent samples t-tests revealed higher disgust in participants exhibiting avoidance behaviors, compared to those with checking behaviors (t(20) = 6.87, p < 0.001). Logistic regression showed that higher disgust scores significantly predicted avoidance behavior (OR = 2.3, 95% CI [1.4, 3.6], p = 0.004).
Reliability and Validity
The internal consistency of the Disgust Sensitivity Scale was high (Cronbach’s α = 0.84), and inter-rater reliability of qualitative coding was acceptable (Cohen’s κ = 0.78). Member checking with selected participants confirmed the accuracy of identified themes. Peer debriefing supported the credibility and confirmability of qualitative results.
Using PQMethod software, three cognitive response patterns were extracted:
- Contamination Sensitivity: aligned with high disgust and avoidance behaviors.
- Safety-Oriented Cognition: associated with control/checking compulsions.
- Order and Predictability Seeking: reflecting structure-focused obsessions.
The fsQCA revealed that high disgust sensitivity in combination with unmarried status and female gender was a consistent configuration leading to compulsive washing (consistency = 0.91; coverage = 0.63). A separate configuration involving high anxiety and marital status explained security-checking behaviors (consistency = 0.87).
Mixed-methods triangulation identified two major subtypes:
Mixed-methods triangulation identified two major subtypes:
- Disgust-dominant subtype: predominantly unmarried females with high contamination sensitivity, characterized by avoidance and washing behaviors.
- Anxiety-driven subtype: primarily married males with heightened security concerns, exhibiting checking compulsions.
Graphical models and integrated factor maps demonstrated strong overlap between disgust-focused responses and compulsive action networks, confirming the convergence of qualitative and quantitative data.
Disgust sensitivity and behavioral responses were moderated by:
Disgust sensitivity and behavioral responses were moderated by:
- Gender roles: females emphasized hygiene, while males leaned toward control.
- Cultural/religious norms: heightened emphasis on ritual cleanliness.
- Family history: early exposure to strict hygiene routines and familial OCD traits increased susceptibility.
Discussion
This study sought to explore the central role of disgust in contamination-based OCD through a mixed-methods approach, integrating qualitative data from semi-structured interviews with quantitative findings from SEM, network analysis, and fsQCA. The results affirmed the hypothesis that disgust is not a peripheral emotion in OCD but functions as a core affective mechanism that significantly drives compulsive behaviors—particularly washing and avoidance—among individuals with this subtype.
Consistent with prior research, a strong association was found between disgust sensitivity and compulsive washing [2, 21]. Disgust intensity was highest among behaviors involving avoidance of contamination and sensitivity to public spaces, supporting previous findings that link disgust to contamination fears and interpersonal avoidance [22]. Neurobiological literature underscores these findings, highlighting the involvement of the insula in disgust processing and its hyperactivation in OCD patients [9, 23].
The SEM and network analysis further revealed that disgust and anxiety interact in reinforcing compulsive behaviors, particularly through feedback loops between emotional reactivity and ritual actions, a concept supported by Berger and Anaki [24]. Cognitive biases, such as selective attention to contamination cues and heightened memory recall of disgusting stimuli, exacerbate the perception of threat [10, 25].
The findings additionally supported the fsQCA model, showing that unmarried women with high disgust sensitivity are most likely to present with washing-related compulsions. These gender differences may be partially attributed to sociocultural norms and role expectations [14, 26]. Religious beliefs, strict childhood hygiene norms, and economic stressors were also identified as contextual modifiers, in line with the law of contagion and culturally reinforced fears [27, 28].
Importantly, this study highlights that disgust demonstrates greater resistance to traditional Exposure and Response Prevention interventions, compared to anxiety, suggesting a need for tailored therapeutic strategies [29]. Emerging modalities, such as imagery rescripting [30] and deep brain stimulation [31], show promise for addressing these limitations.
Despite its strengths, the study had some limitations. First, the sample size was relatively small (N = 30), which may limit the generalizability of quantitative findings. Second, all participants were recruited from clinical settings, possibly skewing responses toward more severe symptomatology. Third, cultural factors were explored in depth but may not be universally generalizable beyond the Iranian context.
Future research should expand to cross-cultural comparisons and longitudinal designs to examine changes in disgust sensitivity over time. The development of disgust-specific therapeutic protocols—potentially integrating cognitive bias modification or targeted neurofeedback—is also recommended. Additional experimental work using neuroimaging could clarify the neural circuits involved in disgust regulation.
Figure 2 presents a conceptual model of how disgust functions as a central driving mechanism in contamination-based OCD. Based on our mixed-methods investigation combining qualitative interviews with advanced quantitative analyses (SEM, network analysis, and fsQCA), the model illustrates the role of disgust not merely as a secondary emotional response but as a fundamental affective component that generates and maintains compulsive behaviors in this OCD subtype.
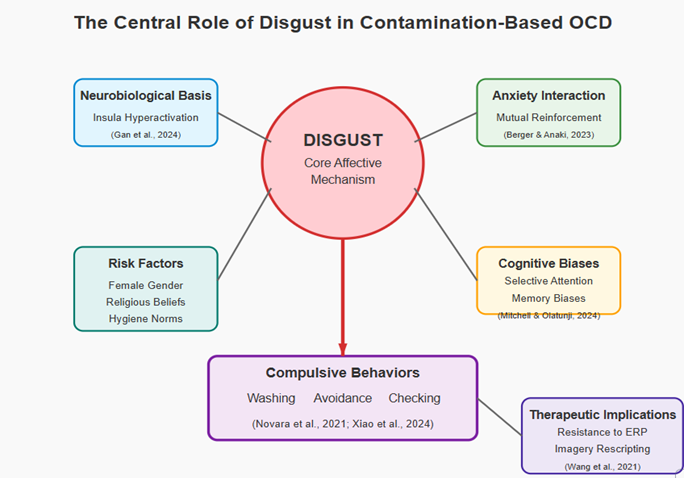
Figure 2. An integrated model of disgust as a core mechanism in contamination-based obsessive-compulsive disorder
Conclusion
This mixed-methods investigation confirms that disgust plays a central, multifactorial role in contamination-based OCD. Unlike anxiety-driven subtypes, individuals with contamination concerns exhibit intense, persistent disgust responses that drive compulsive rituals and resist traditional treatments. The integrative model of this study incorporates emotional, cognitive, biological, and sociocultural factors, offering a comprehensive framework for clinical assessment and intervention. Addressing disgust directly, both psychologically and neurologically, may represent the next frontier in treating this pervasive and impairing disorder.
Ethical Considerations
The study protocol was reviewed and approved by the Royan Institute Ethics Committee under code IR.ACECR.ROYAN.REC.1401.063. All participants provided written informed consent after receiving a full explanation of study objectives, procedures, risks, and rights, including the right to withdraw without penalty. Data were anonymized, encrypted, and stored securely in accordance with international ethical guidelines for research involving human subjects.
Acknowledgments
The authors would like to express their sincere gratitude to all participants who generously shared their time and experiences, making this research possible. We also thank the clinical centers and professionals who supported the recruitment and assessment process. Appreciation is extended to colleagues and peer reviewers whose insights contributed to the refinement of this work. No specific funding was received for this study.
Authors' Contributions
All authors contributed substantially to the conception and design of the study, acquisition and interpretation of data, and drafting or revising the manuscript. All authors read and approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Funding/Support
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
This mixed-methods investigation confirms that disgust plays a central, multifactorial role in contamination-based OCD. Unlike anxiety-driven subtypes, individuals with contamination concerns exhibit intense, persistent disgust responses that drive compulsive rituals and resist traditional treatments. The integrative model of this study incorporates emotional, cognitive, biological, and sociocultural factors, offering a comprehensive framework for clinical assessment and intervention. Addressing disgust directly, both psychologically and neurologically, may represent the next frontier in treating this pervasive and impairing disorder.
Ethical Considerations
The study protocol was reviewed and approved by the Royan Institute Ethics Committee under code IR.ACECR.ROYAN.REC.1401.063. All participants provided written informed consent after receiving a full explanation of study objectives, procedures, risks, and rights, including the right to withdraw without penalty. Data were anonymized, encrypted, and stored securely in accordance with international ethical guidelines for research involving human subjects.
Acknowledgments
The authors would like to express their sincere gratitude to all participants who generously shared their time and experiences, making this research possible. We also thank the clinical centers and professionals who supported the recruitment and assessment process. Appreciation is extended to colleagues and peer reviewers whose insights contributed to the refinement of this work. No specific funding was received for this study.
Authors' Contributions
All authors contributed substantially to the conception and design of the study, acquisition and interpretation of data, and drafting or revising the manuscript. All authors read and approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Funding/Support
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Wu MS, Storch EA. A case report of harm-related obsessions in pediatric obsessive-compulsive disorder. J Clin Psychol. 2016;72(11):1120-1128. [DOI: 10.1002/jclp.22392. Epub 2016 Sep 18] [PMID]
- Novara C, Lebrun C, Macgregor A, Vivet B, Thérouanne P, Capdevielle D, Raffard S. Acquisition and maintenance of disgust reactions in an OCD analogue sample: Efficiency of extinction strategies through a counter-conditioning procedure. PLoS One. 2021;16(7):e0254592. [DOI:10.1371/journal.pone.0254592] [PMID] [PMCID]
- Buyukturkoglu K, Roettgers H, Sommer J, Rana M, Dietzsch L, Arikan EB, Veit R, Malekshahi R, Kircher T, Birbaumer N, Sitaram R, Ruiz S. Self-regulation of anterior insula with real-time fmri and its behavioral effects in obsessive-compulsive disorder: a feasibility study. PLoS One. 2015;10(8):e0135872. [DOI:10.1371/journal.pone.0135872] [PMID] [PMCID]
- Karthik S, Sharma LP, Narayanaswamy JC. Investigating the role of glutamate in obsessive-compulsive disorder: current perspectives. Neuropsychiatr Dis Treat. 2020;16:1003-1013. [DOI: 10.2147/NDT.S211703] [PMID] [PMCID]
- Xu J, Hao Q, Qian R, Mu X, Dai M, Wu Y, et al. Optimal dose of serotonin reuptake inhibitors for obsessive-compulsive disorder in adults: a systematic review and dose-response meta-analysis. Front Psychiatry. 2021;12:717999. [ DOI: 10.3389/fpsyt.2021.717999] [PMID][PMCID]
- Blanco-Vieira T, Radua J, Marcelino L, Bloch M, Mataix-Cols D, Do Rosário MC. The genetic epidemiology of obsessive-compulsive disorder: a systematic review and meta-analysis. Transl Psychiatry. 2023;13(1):230. [DOI: 10.1038/s41398-023-02433-2] [PMID][PMCID]
- Hodny F, Ociskova M, Prasko J, Vanek J, Visnovsky J, Sollar T, Slepecky M, et al. Early life experiences and adult attachment in obsessive-compulsive disorder. Part 2: Therapeutic effectiveness of combined cognitive behavioural therapy and pharmacotherapy in treatment-resistant inpatients. Neuro Endocrinol Lett. 2022;43(6):345-358. [PMID]
- Ameli P, Babakhani A, Oliver DS. 28-year-old woman• weakness• anxiety• altered mental status• Dx?. J Fam Pract. 2020; 69(8):412-3.[ PMID]
- Gan X, Zhou F, Xu T, Liu X, Zhang R, Zheng Z, et al. A neurofunctional signature of subjective disgust generalizes to oral distaste and socio-moral contexts. Nat Hum Behav. 2024;8(7):1383-1402. [DOI: 10.1038/s41562-024-01868-x] [PMID]
- Knowles KA, Cox RC, Armstrong T, Olatunji BO. Cognitive mechanisms of disgust in the development and maintenance of psychopathology: A qualitative review and synthesis. Clin Psychol Rev. 2019;69:30-50. [DOI:10.1016/j.cpr.2018.06.002] [PMID] [PMCID]
- Seyedmirzaei H, Bayan N, Ohadi MAD, Cattarinussi G, Sambataro F. Effects of antidepressants on brain structure and function in patients with obsessive-compulsive disorder: A review of neuroimaging studies. Psychiatry Res Neuroimaging. 2024;342:111842. [DOI:10.1016/j.pscychresns.2024.111842] [PMID]
- Zhao YJ, Zhang Y, Wang Q, Manssuer L, Cui H, Ding Q, Sun B, Liu W, Voon V. Evidence accumulation and neural correlates of uncertainty in obsessive-compulsive disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2023 ;8(10):1058-1065. [DOI: 10.1016/j.bpsc.2023.05.011] [PMID] [PMCID]
- Demaria F, Pontillo M, Di Vincenzo C, Di Luzio M, Vicari S. Hand Washing: When ritual behavior protects! obsessive-compulsive symptoms in young people during the COVID-19 pandemic: A narrative review. J Clin Med. 2022;11(11):3191. [DOI: 10.3390/jcm11113191] [PMID] [PMCID]
- Rosa-Alcázar AI, Iniesta-Sepúlveda M. Integrating family therapy into exposure-based CBT for a Spanish patient with obsessive scrupulosity. Bull Menninger Clin. 2018;82(4):308-325. [DOI:10.1521/bumc.2018.82.4.308] [PMID]
- Jalal B, Chamberlain SR, Sahakian BJ. Obsessive-compulsive disorder: Etiology, neuropathology, and cognitive dysfunction. Brain Behav. 2023;13(6):e3000. [DOI: 10.1002/brb3.3000] [PMID] [PMCID]
- Knowles KA, Olatunji BO. Anxiety and safety behavior usage during the COVID-19 pandemic: the prospective role of contamination fear. J Anxiety Disord. 2021;77:102323. [DOI:10.1016/j.janxdis.2020.102323] [PMID] [PMCID]
- Vogt GS, Avendaño-Ortega M, Schneider SC, Goodman WK, Storch EA. Optimizing obsessive-compulsive symptom measurement with the yale-brown obsessive-compulsive scales-second edition. J Psychiatr Pract. 2022;28(4):294-309. [DOI:10.1097/PRA.0000000000000640] [PMID] [PMCID]
- Gonçalves T, Curado C, Balle AR. Psychosocial antecedents of knowledge sharing in healthcare research centers: a mixed-methods approach. J Health Organ Manag. 2021;ahead-of-print(ahead-of-print). [DOI: 10.1108/JHOM-12-2020-0463] [PMID]
- Abegglen S, Krieg A, Eigenmann H, Greif R. Objective structured assessment of debriefing (OSAD) in simulation-based medical education: Translation and validation of the German version. PLoS One. 2020 31;15(12):e0244816. [DOI:10.1371/journal.pone.0244816] [PMID] [PMCID]
- Ali N MSc, PT, May S PhD, PT, Grafton K PhD, PT. A systematic review of grounded theory studies in physiotherapy. Physiother Theory Pract. 2019;35(12):1139-1169. [DOI:10.1080/09593985.2018.1474403] [PMID]
- Xiao Q, Hou J, Xiao L, Zhou M, He Z, Dong H, Hu S. Lower synaptic density and its association with cognitive dysfunction in patients with obsessive-compulsive disorder. Gen Psychiatr. 2024;37(3):e101208. [DOI:10.1136/gpsych-2023-101208] [PMID] [PMCID]
- Söylemez S, Kapucu A. The impact of disgust learning on memory processes for neutral stimuli: a classical conditioning approach. Cogn Emot. 2025;39(2):339-354. [DOI: 10.1080/02699931.2024.2413359] [PMID]
- Gkintoni E, Ortiz PS. Neuropsychology of generalized anxiety disorder in clinical setting: A systematic evaluation. Healthcare (Basel). 2023;11(17):2446. [DOI:10.3390/healthcare11172446] [PMID] [PMCID]
- Berger U, Anaki D. Exploring the role of the self in disgust-related psychopathologies. Bull Menninger Clin. 2023;87(Supplement A):113-132. [DOI: 10.1521/bumc.2023.87.suppA.113] [PMID]
- Mitchell BJ, Olatunji BO. State of the science: disgust and the anxiety disorders. Behav Ther. 2024;55(6):1144-1157. [DOI:10.1016/j.beth.2024.02.005] [PMID]
- Mitchell BJ, Olatunji BO. State of the science: disgust and the anxiety disorders. Behav Ther. 2024;55(6):1144-1157. [DOI:10.1016/j.beth.2024.02.005] [PMID]
- Crookes DM, Lemon ED, Sainz M, Del Carmen Chacón L, Urbina BM, Woods-Jaeger B. Immigration enforcement climate in Georgia and the mental health of Latinx immigrants. J Health Care Poor Underserved. 2023;34(2):798-809. [DOI:10.1353/hpu.2023.0041] [PMID] [PMCID]
- Eyal T, Dar R, Liberman N. Is disgust in obsessive-compulsive disorder mediated by fear of pathogens?. J Anxiety Disord. 2021;77:102340. [DOI:10.1016/j.janxdis.2020.102340] [PMID]
- Keleher J, Jassi A, Krebs G. Clinician-reported barriers to using exposure with response prevention in the treatment of paediatric obsessive-compulsive disorder. J Obsessive Compuls Relat Disord. 2020;24:100498. [DOI: 10.1016/j.jocrd.2019.100498] [PMID] [PMCID]
- Wang J, Sun X, Lu J, Dou H, Lei Y. Generalization gradients for fear and disgust in human associative learning. Sci Rep. 2021;11(1):14210. [DOI:10.1038/s41598-021-93544-7] [PMID] [PMCID]
- Yan H, Elkaim LM, Venetucci Gouveia F, Huber JF, Germann J, Loh A, et al. Deep brain stimulation for extreme behaviors associated with autism spectrum disorder converges on a common pathway: a systematic review and connectomic analysis. J Neurosurg. 2022;137(3):699-708. [DOI:10.3171/2021.11.JNS21928] [PMID]
Article Type: Research Article |
Subject:
Anxiety and Stress
Received: 2025/04/21 | Accepted: 2025/06/17 | Published: 2025/07/19
Received: 2025/04/21 | Accepted: 2025/06/17 | Published: 2025/07/19
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |