Volume 10, Issue 1 (February 2023)
Avicenna J Neuro Psycho Physiology 2023, 10(1): 34-40 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kabunga A, Kigongo E, Musinguzi M, Tumwesigye R, Acup W. A systematic review and meta-analysis of the prevalence of depression among breast cancer patients in Sub-Saharan Africa. Avicenna J Neuro Psycho Physiology 2023; 10 (1) :34-40
URL: http://ajnpp.umsha.ac.ir/article-1-449-en.html
URL: http://ajnpp.umsha.ac.ir/article-1-449-en.html
1- Department of Psychiatry, Lira University, Northern Uganda , akabunga@lirauni.ac.ug
2- Department of Environmental Health and Disease Control, Lira University, Northern Uganda
3- Department of Community Health, Northern Uganda
4- Department of Nursing, Lira University, Northern Uganda
2- Department of Environmental Health and Disease Control, Lira University, Northern Uganda
3- Department of Community Health, Northern Uganda
4- Department of Nursing, Lira University, Northern Uganda
Full-Text [PDF 1772 kb]
(674 Downloads)
| Abstract (HTML) (2657 Views)
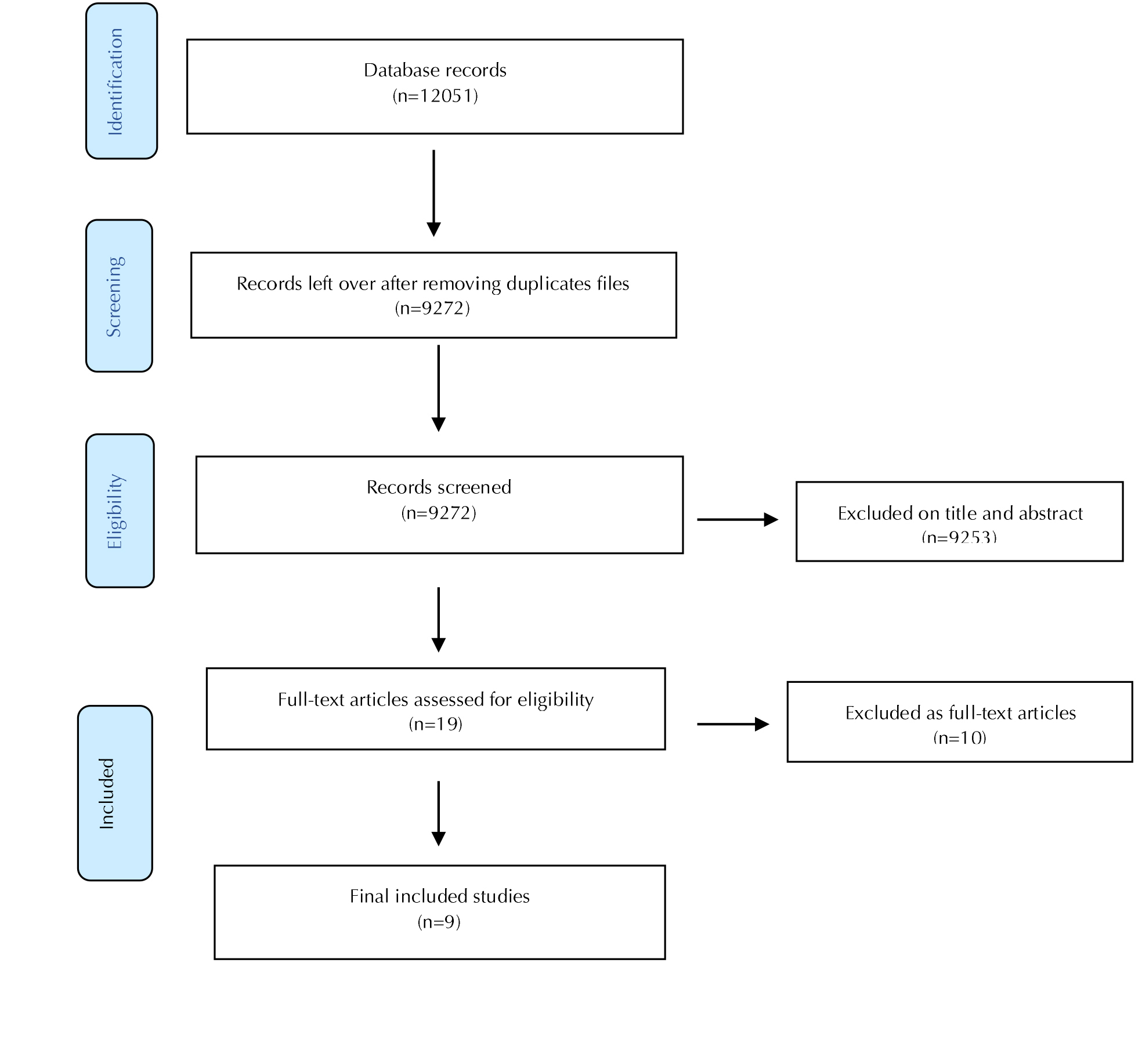
Figure 1. Flow chart for the selection process
Table 1. Characteristics of the studies included
CI: Confidence interval; LCI: Lower confidence interval; UCI: Upper confidence interval; HADS: Hospital Anxiety and Depression scale; PHQDAS: Patient Health Questionnaire and Depression Anxiety Stress Scale; PHQ 9: Patient Health Questionnaire 9; CESDS: Center for Epidemiological Studies-Depression scale, HSC: Hopkins Symptom checklist
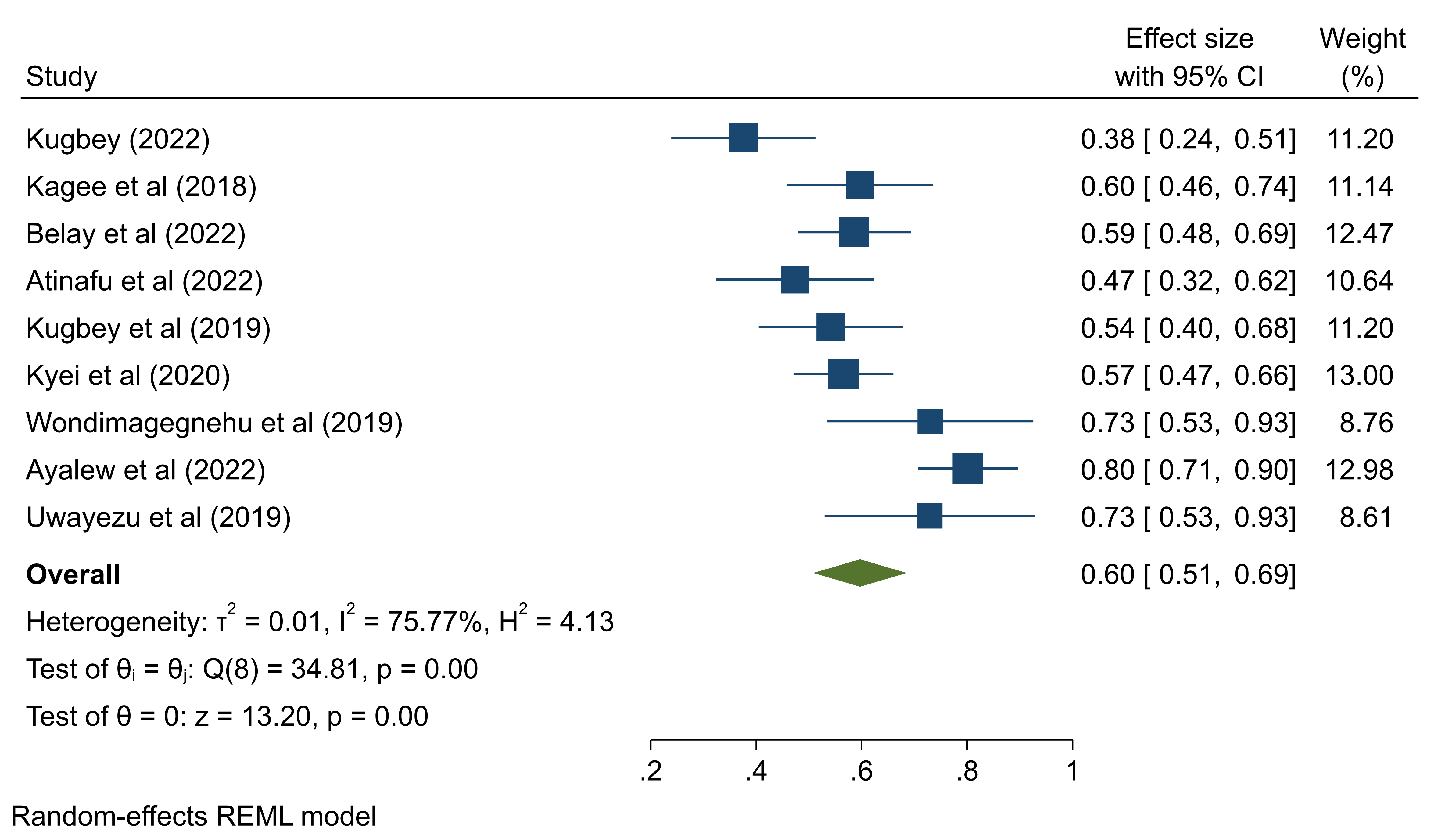
Figure 2. Forest plot demonstrating the pooled prevalence of depression among breast cancer patients in Sub-Saharan Africa
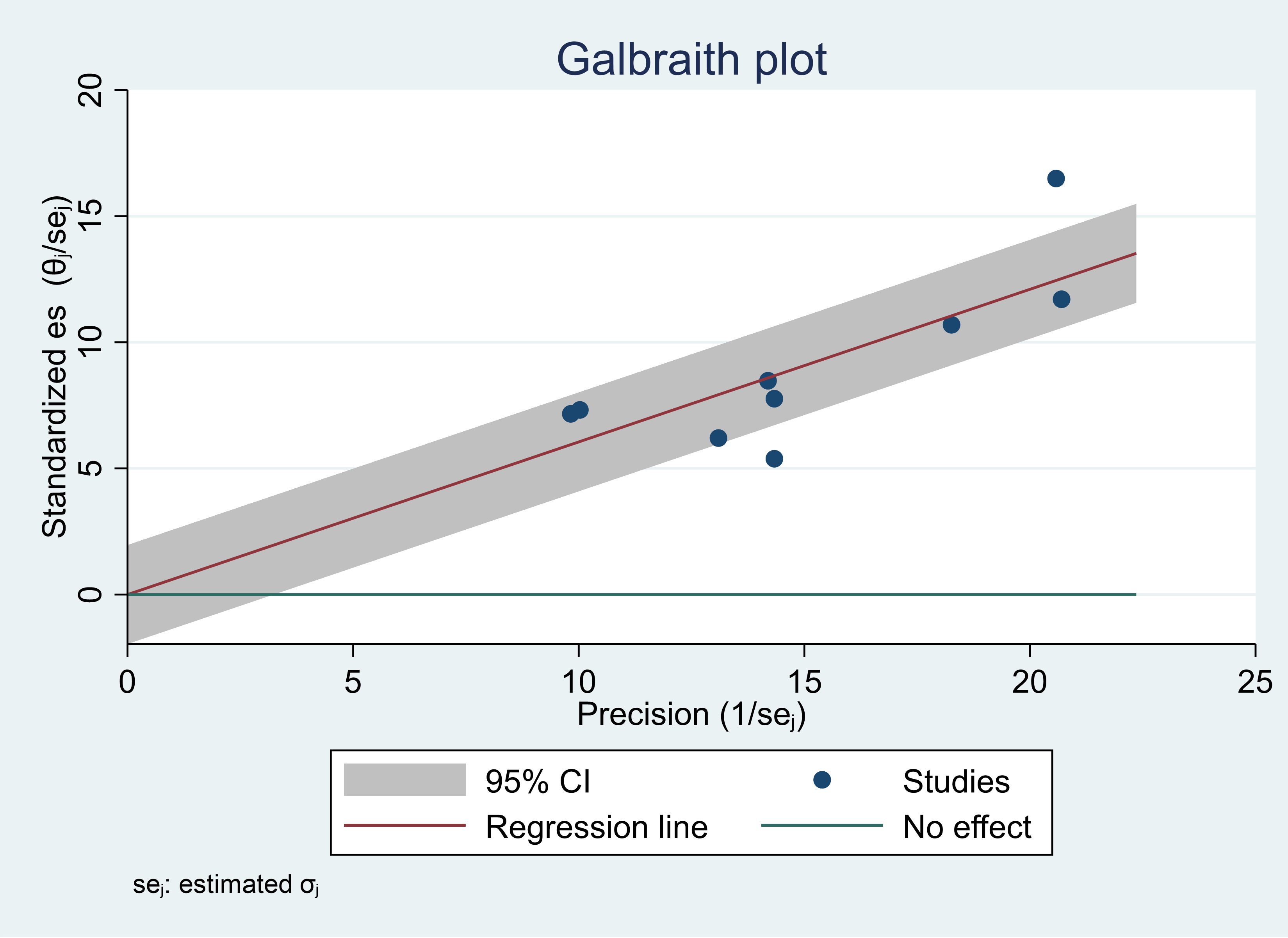
Figure 3. Galbraith plot showing heterogeneity among included studies for the prevalence of depression among breast cancer patients in Sub-Saharan Africa
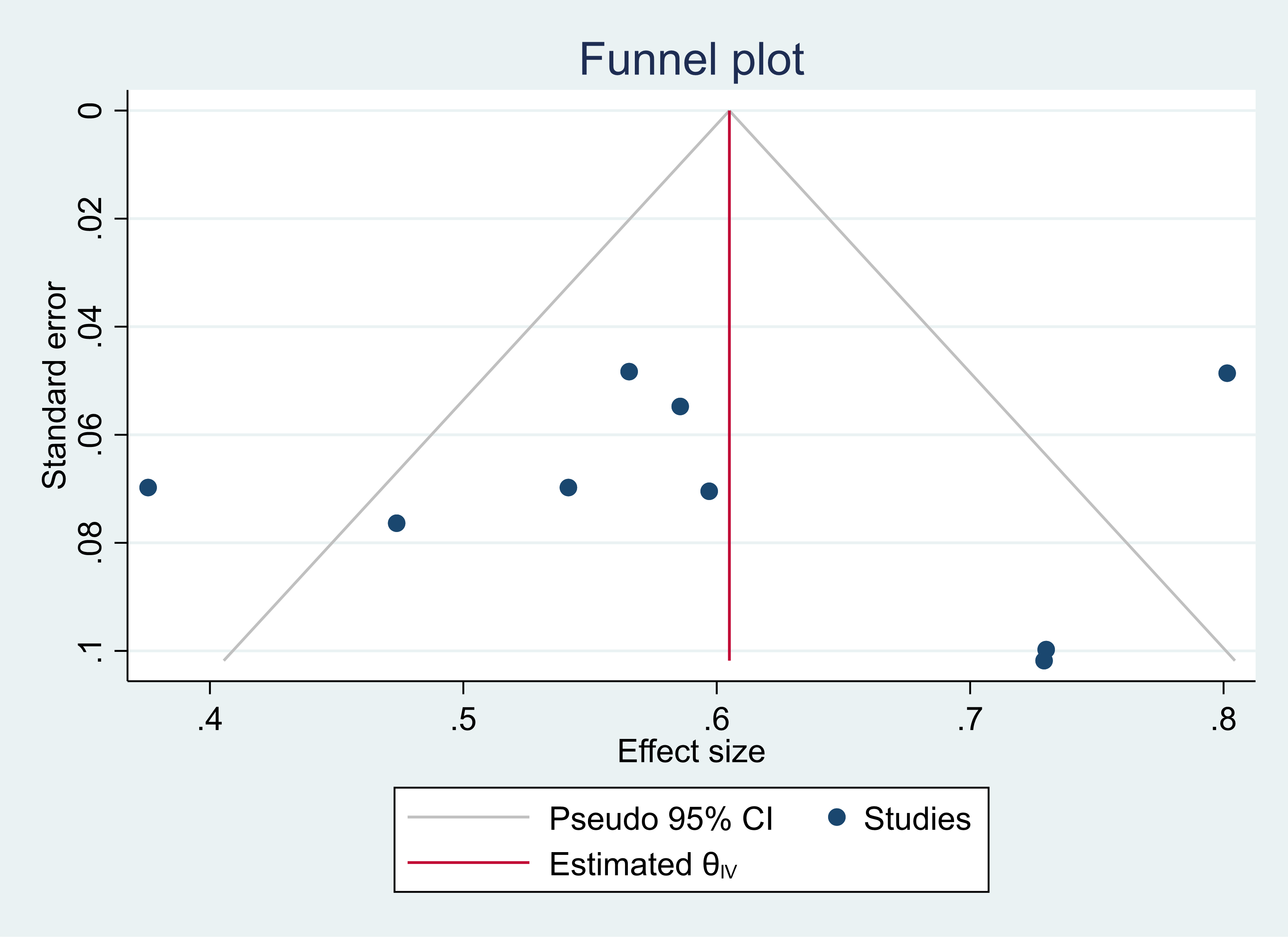
Figure 4. Funnel plot showing the absence of potential publication bias
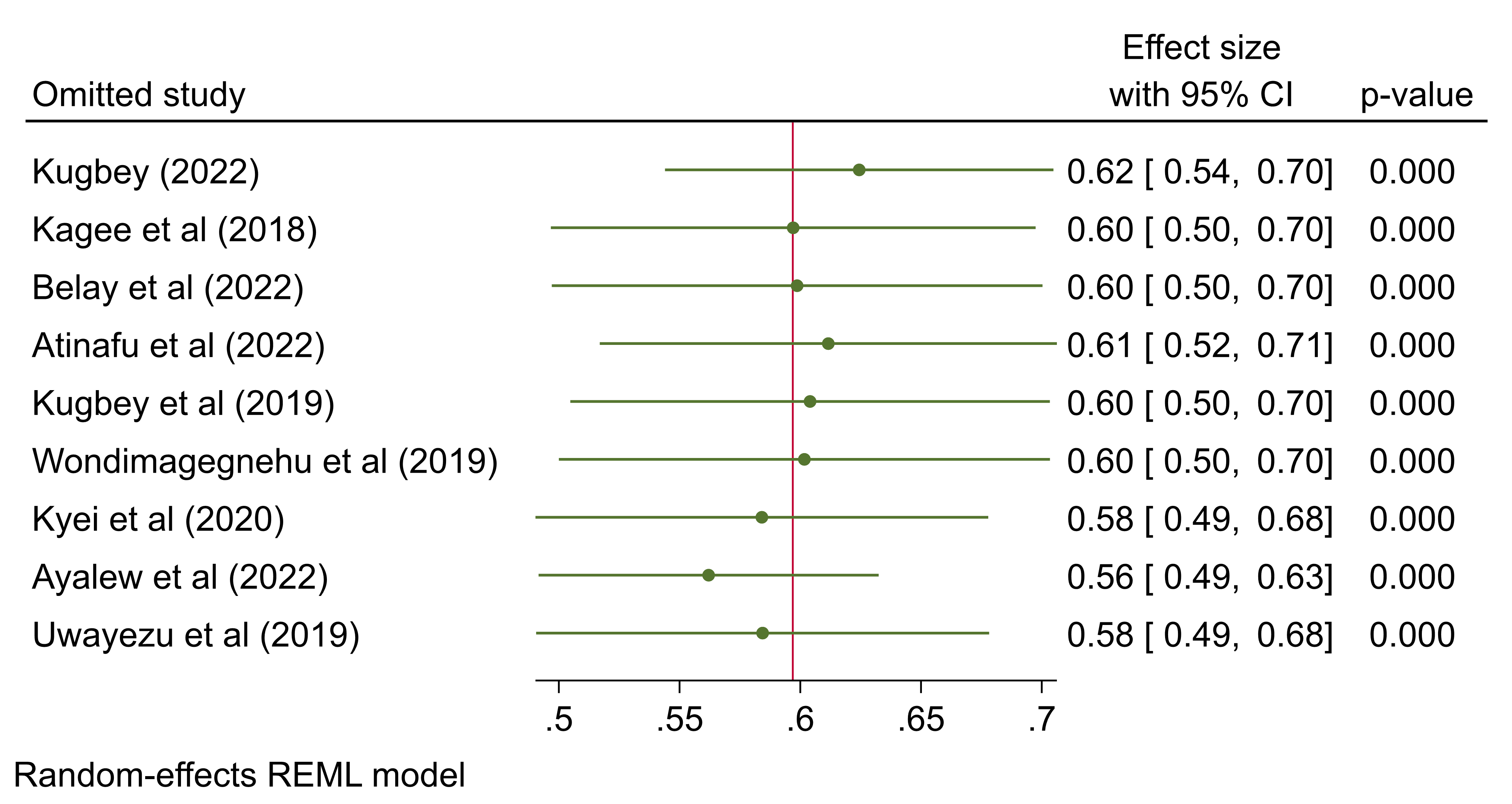
Figure 5. Forest plot showing leave one out sensitivity analysis
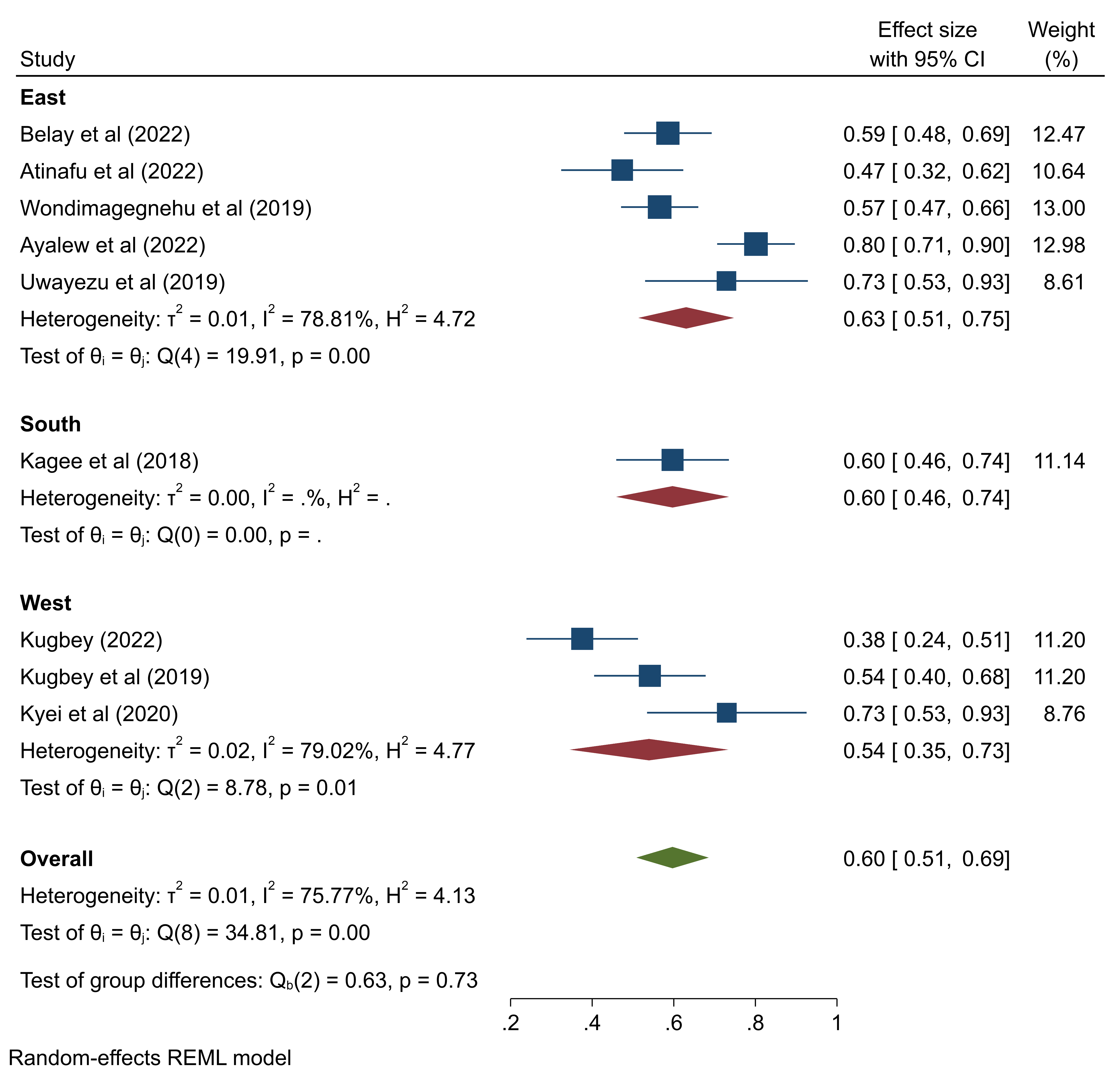
Figure 6. Forest plot showing the pooled prevalence of depression among breast cancer patients in Sub-Saharan Africa by region
Full-Text: (1260 Views)
Background
One of the problems facing health systems today is cancer. One in eight women worldwide will develop breast cancer [1]. With a global incidence of 11.6%, breast cancer accounted for 6.5% of all cancer deaths in 2019 [2]. Furthermore, by 2046, there will be 3 million new cases of breast cancer, from 2 million in 2018—a 46% increase [3]. Breast cancer is the most common form of cancer diagnosed worldwide and the leading cause of death in more than one hundred countries [4]. The death rate from breast cancer is still high despite improvements in early detection and treatment [5].
Based on the studies, the prevalence of depression in breast cancer patients ranged from 9.3%-56% [6,7]. According to a meta-analysis, 32.2% of cancer patients experience depression. A meta-analysis revealed that the prevalence of depression among cancer patients was 32.2% [1]. To improve the chances of breast cancer patients' survival and reduce their mortality, it is crucial to identify the related risk factors [8]. Depression can both shorten and predict the survival time of cancer patients [9].
Previous studies demonstrated that people with a cancer diagnosis have a significant level of depression [10]. These studies, however, have focused on a specific type of breast cancer [1], with no perspective from Sub-Saharan Africa.
Policymakers can benefit from knowing the true extent of depression in the region so they can take more effective preventative measures. In light of the aforementioned issues, the present study aimed to address this knowledge gap by determining the prevalence of depression among those dealing with breast cancer in Sub-Saharan Africa.
Objectives
To assess the combined prevalence of breast cancer-related depression among patients in Sub-Saharan Africa.
Materials and Methods
Design
This systematic review synthesized evidence on breast cancer depression in Sub-Saharan Africa. The study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [11] and was registered with PROSPERO (NO: CRD42022374481).
Search methods
We searched published papers from PubMed, Web of Science, Science Direct, African Journals Online, and Google Scholar from January 2012 to December 2022. We also searched for gray literature from reports and unpublished work. In order to avoid omitting other articles, reference lists from conducted systematic reviews were searched. A combination of key terms of depression, depressive disorders, breast cancer, mammary cancer, mammary adenocarcinoma, and breast carcinoma, Sub-Saharan Africa using Boolean operators to create a search query in different databases. The searched articles were reviewed between November and December 2022.
Selection criteria
Only primary studies reporting on depression among breast cancer patients in Sub-Saharan African countries and published in English over the past decade were included in the analysis (January 2012 to December 2022). Letters to the editor, conference proce1edings, editorials, policy publications, retracted papers, and reviews were not included in the review. In addition, duplicate studies were not included in the analysis.
Study selection
Studies were independently entered into Endnote X9 for screening from all databases. Before the actual screening, a command was run to remove all duplicate files. Two independent reviewers (AK and EK) screened studies using the inclusion and exclusion criteria as a guide for the quality of the selection process. The final decision on whether to include or exclude the study in question was left up to a third reviewer (MM) in cases where the first two reviewers were unable to reach an agreement on the studies.
Search outcome
After the elimination of duplicates, 9272 articles were still found after the electronic search yielded 12051 results. A number of 19 articles were still available after abstract and title screening, and they underwent full-text screening. A number of 10 articles were removed due to incomplete reporting of their full outcome of interest (n=6), incorrect publication type (n=2), and lack of full-text availability (n=6). The outcomes are displayed in Figure 1.
Based on the studies, the prevalence of depression in breast cancer patients ranged from 9.3%-56% [6,7]. According to a meta-analysis, 32.2% of cancer patients experience depression. A meta-analysis revealed that the prevalence of depression among cancer patients was 32.2% [1]. To improve the chances of breast cancer patients' survival and reduce their mortality, it is crucial to identify the related risk factors [8]. Depression can both shorten and predict the survival time of cancer patients [9].
Previous studies demonstrated that people with a cancer diagnosis have a significant level of depression [10]. These studies, however, have focused on a specific type of breast cancer [1], with no perspective from Sub-Saharan Africa.
Policymakers can benefit from knowing the true extent of depression in the region so they can take more effective preventative measures. In light of the aforementioned issues, the present study aimed to address this knowledge gap by determining the prevalence of depression among those dealing with breast cancer in Sub-Saharan Africa.
Objectives
To assess the combined prevalence of breast cancer-related depression among patients in Sub-Saharan Africa.
Materials and Methods
Design
This systematic review synthesized evidence on breast cancer depression in Sub-Saharan Africa. The study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [11] and was registered with PROSPERO (NO: CRD42022374481).
Search methods
We searched published papers from PubMed, Web of Science, Science Direct, African Journals Online, and Google Scholar from January 2012 to December 2022. We also searched for gray literature from reports and unpublished work. In order to avoid omitting other articles, reference lists from conducted systematic reviews were searched. A combination of key terms of depression, depressive disorders, breast cancer, mammary cancer, mammary adenocarcinoma, and breast carcinoma, Sub-Saharan Africa using Boolean operators to create a search query in different databases. The searched articles were reviewed between November and December 2022.
Selection criteria
Only primary studies reporting on depression among breast cancer patients in Sub-Saharan African countries and published in English over the past decade were included in the analysis (January 2012 to December 2022). Letters to the editor, conference proce1edings, editorials, policy publications, retracted papers, and reviews were not included in the review. In addition, duplicate studies were not included in the analysis.
Study selection
Studies were independently entered into Endnote X9 for screening from all databases. Before the actual screening, a command was run to remove all duplicate files. Two independent reviewers (AK and EK) screened studies using the inclusion and exclusion criteria as a guide for the quality of the selection process. The final decision on whether to include or exclude the study in question was left up to a third reviewer (MM) in cases where the first two reviewers were unable to reach an agreement on the studies.
Search outcome
After the elimination of duplicates, 9272 articles were still found after the electronic search yielded 12051 results. A number of 19 articles were still available after abstract and title screening, and they underwent full-text screening. A number of 10 articles were removed due to incomplete reporting of their full outcome of interest (n=6), incorrect publication type (n=2), and lack of full-text availability (n=6). The outcomes are displayed in Figure 1.
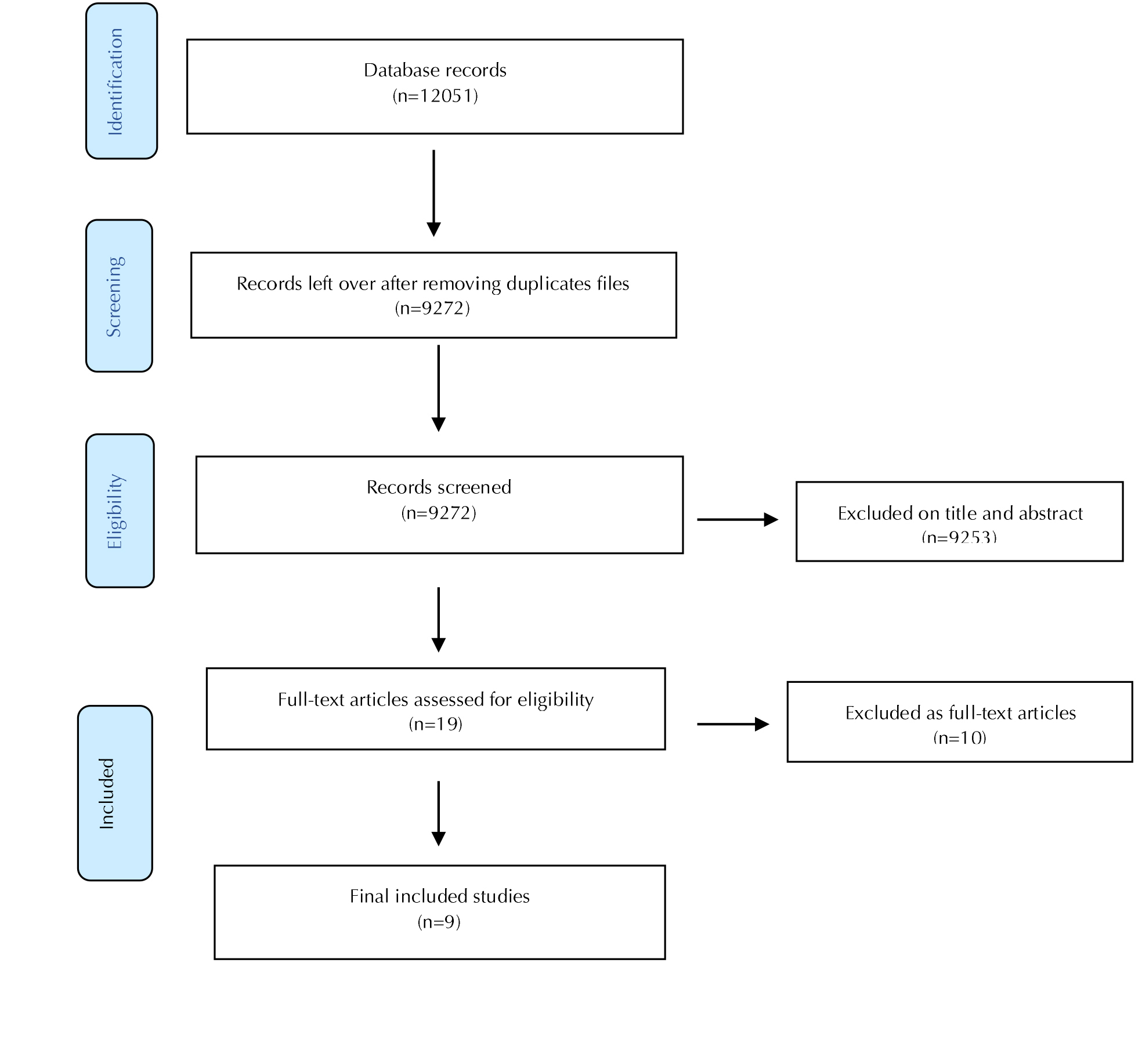
Figure 1. Flow chart for the selection process
Data collection
Data extraction from the included articles was carried out by two independent reviewers (WA and MM), and the gathered data was jointly verified. The first author's name, the publication date, the journal, the country and region, the sample size, age, gender, the study period, the incidence of depression score and prevalence, as well as other pertinent data, were all gathered using a Microsoft Excel 2013 template.
Quality of included studies
Studies with a high quality of bias (a score of 5-9) were disqualified from the final analysis. The quality of the included studies was assessed using the Newcastle-Ottawa Scale. To ensure consistency, the evaluation was conducted sequentially by two reviewers (WA and RT). If disagreements arose, they were talked out with a third reviewer (AK).
Statistical analysis
The data were analyzed in STATA version 17 (StataCorp, College Station, Texas, USA) using the metaan command. Before deciding to combine the included studies, a clinical assessment of individual studies was conducted on the study outcomes and the quality of the study, among other characteristics. Due to high heterogeneity (above 50%), a random-effects model with a 95% confidence interval was utilized to determine breast cancer depression levels among breast cancer patients combined from the
included studies. Publication bias was evaluated using Egger's test and funnel plot asymmetry, demonstrating a potential publication bias due to small study effects. A sensitivity analysis was conducted to assess the robustness of the results based on the potential causes of bias. In addition, the quality of evidence for clinical significance was assessed using the Grades of Recommendation, Assessment, Development, and Evaluation system [13]. Sub-group analysis was performed based on the potential sources of bias identified.
Results
Out of the 1,2051 retrieved articles, 9 studies from West Africa(n=3), East Africa(n=5), and South Africa(n=1) were incorporated into the final analysis. A total of 2162 participants, ranging in size from 96-423, made up the sample. Patients with a breast cancer diagnosis, regardless of stage, were eligible to participate. The most recent survey was conducted on September 2022, and the first survey was conducted between January and December 2017. Each cross-sectional study was released between 2012 and 2022. A low risk of bias existed for the vast majority of the studies included (Table 1).
Pooled prevalence of depression
The pooled prevalence of breast cancer patients in Sub-Saharan Africa was 60%(95%CI, 0.51-0.69) using a random-effects model (Figure 2).
Data extraction from the included articles was carried out by two independent reviewers (WA and MM), and the gathered data was jointly verified. The first author's name, the publication date, the journal, the country and region, the sample size, age, gender, the study period, the incidence of depression score and prevalence, as well as other pertinent data, were all gathered using a Microsoft Excel 2013 template.
Quality of included studies
Studies with a high quality of bias (a score of 5-9) were disqualified from the final analysis. The quality of the included studies was assessed using the Newcastle-Ottawa Scale. To ensure consistency, the evaluation was conducted sequentially by two reviewers (WA and RT). If disagreements arose, they were talked out with a third reviewer (AK).
Statistical analysis
The data were analyzed in STATA version 17 (StataCorp, College Station, Texas, USA) using the metaan command. Before deciding to combine the included studies, a clinical assessment of individual studies was conducted on the study outcomes and the quality of the study, among other characteristics. Due to high heterogeneity (above 50%), a random-effects model with a 95% confidence interval was utilized to determine breast cancer depression levels among breast cancer patients combined from the
included studies. Publication bias was evaluated using Egger's test and funnel plot asymmetry, demonstrating a potential publication bias due to small study effects. A sensitivity analysis was conducted to assess the robustness of the results based on the potential causes of bias. In addition, the quality of evidence for clinical significance was assessed using the Grades of Recommendation, Assessment, Development, and Evaluation system [13]. Sub-group analysis was performed based on the potential sources of bias identified.
Results
Out of the 1,2051 retrieved articles, 9 studies from West Africa(n=3), East Africa(n=5), and South Africa(n=1) were incorporated into the final analysis. A total of 2162 participants, ranging in size from 96-423, made up the sample. Patients with a breast cancer diagnosis, regardless of stage, were eligible to participate. The most recent survey was conducted on September 2022, and the first survey was conducted between January and December 2017. Each cross-sectional study was released between 2012 and 2022. A low risk of bias existed for the vast majority of the studies included (Table 1).
Pooled prevalence of depression
The pooled prevalence of breast cancer patients in Sub-Saharan Africa was 60%(95%CI, 0.51-0.69) using a random-effects model (Figure 2).
Table 1. Characteristics of the studies included
| Author | Region | Design | Sampling | Study period | Sample | Depression (n) | Prevalence (95% CI) | Depression tool | Risk |
| Kugbey (2022)[14] | West | Cross-sectional | Simple | Sept 2022 | 205 | 77 | 38(31, 45) | HADS | Low |
| Kagee et al. (2018)[15] | South | Cross-sectional | Convenience | April 2017 | 201 | 120 | 60(53, 67) | CESDS, HSC | Low |
| Belay et al. (2022)[16] | East | Cross-sectional | Simple | March-Sept, 2019 | 333 | 195 | 59(53, 64) | HADS | Low |
| Atinafu et al (2022) [17] | East | Cross-sectional | Consecutive | Dec 2021 | 171 | 81 | 47(40, 55) | HADS | low |
| Kugbey et al. (2019) [18] | West | Cross-sectional | Convenience | June 2019 | 205 | 111 | 54(47, 61) | HADS | Low |
| Wondimagegnehu et al. (2019) [19] | East | Cross-sectional | Not reported | Dec-2017, May 2018 | 428 | 242 | 57(52, 61) | PHQ 9 | Low |
| Kyei et al. (2020) [20] | West | Cross-sectional | Not reported | June-Aug, 2017 | 100 | 73 | 73(63, 81) | PHQDAS | Low |
| Ayalew et al. (2022) [21] | East | Cross-sectional | Simple | Oct-Dec, 2019 | 423 | 339 | 80(76, 84) | HADS | Low |
| Uwayezu et al. (2019) [22] | East | Cross-sectional | Systematic | April-May, 2017 | 96 | 70 | 73(63, 81) | HADS | Low |
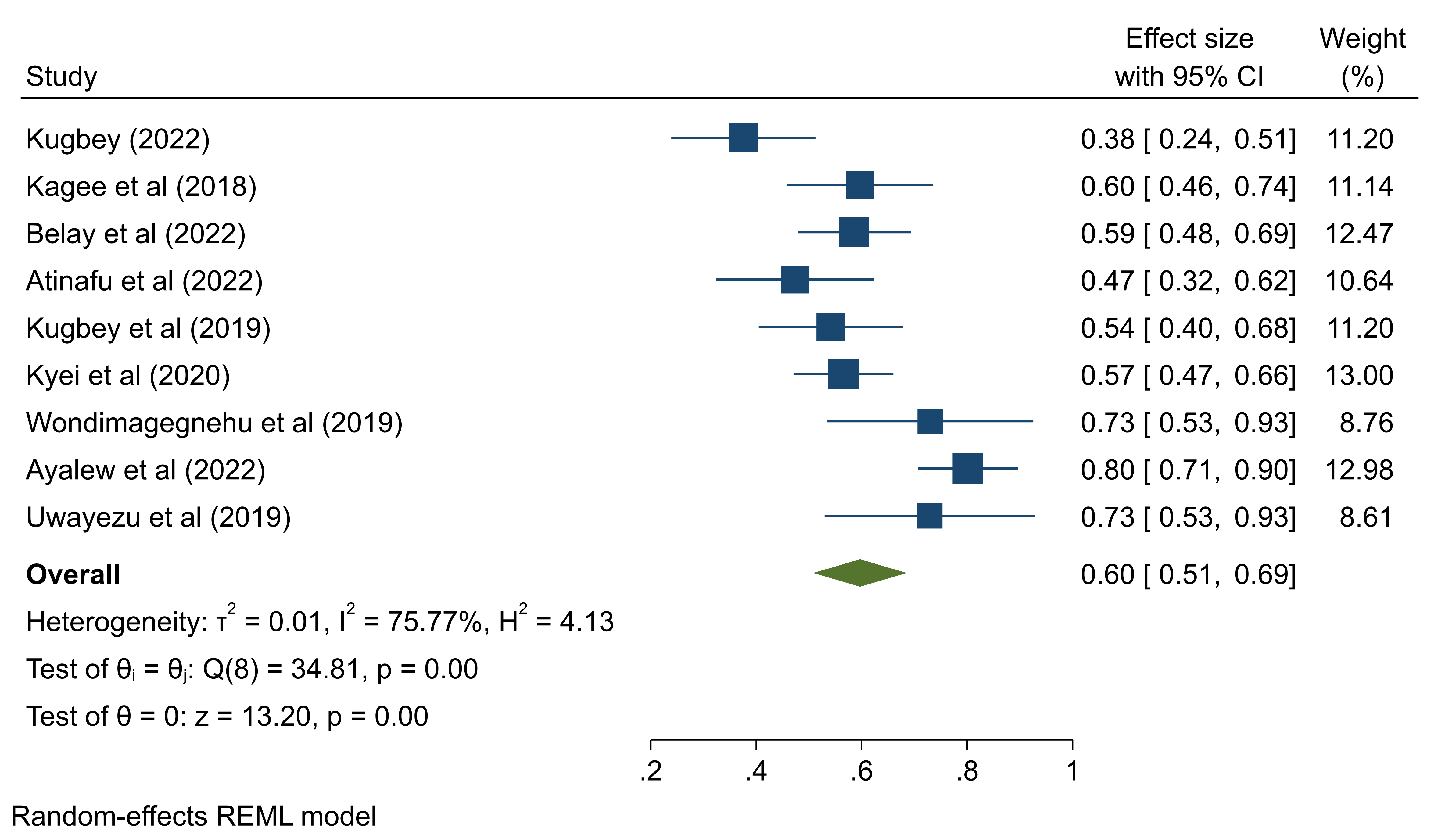
Figure 2. Forest plot demonstrating the pooled prevalence of depression among breast cancer patients in Sub-Saharan Africa
Heterogeneity among selected studies
As displayed in Figure 3 (Galbraith plot), less than 95% of the included studies are within the confidence interval indicating the presence of heterogeneity.
The heterogeneity index (I2) of 75.77%, as depicted in Figure 2, indicates a high hetero-geneity among the included studies [23].
Publication bias
There is no potential publication bias after the observation of funnel plot symmetry (Figure 4). The regression-based Eggers test also shows no small study effects (Z=0.24, p=0.81).
As displayed in Figure 3 (Galbraith plot), less than 95% of the included studies are within the confidence interval indicating the presence of heterogeneity.
The heterogeneity index (I2) of 75.77%, as depicted in Figure 2, indicates a high hetero-geneity among the included studies [23].
Publication bias
There is no potential publication bias after the observation of funnel plot symmetry (Figure 4). The regression-based Eggers test also shows no small study effects (Z=0.24, p=0.81).
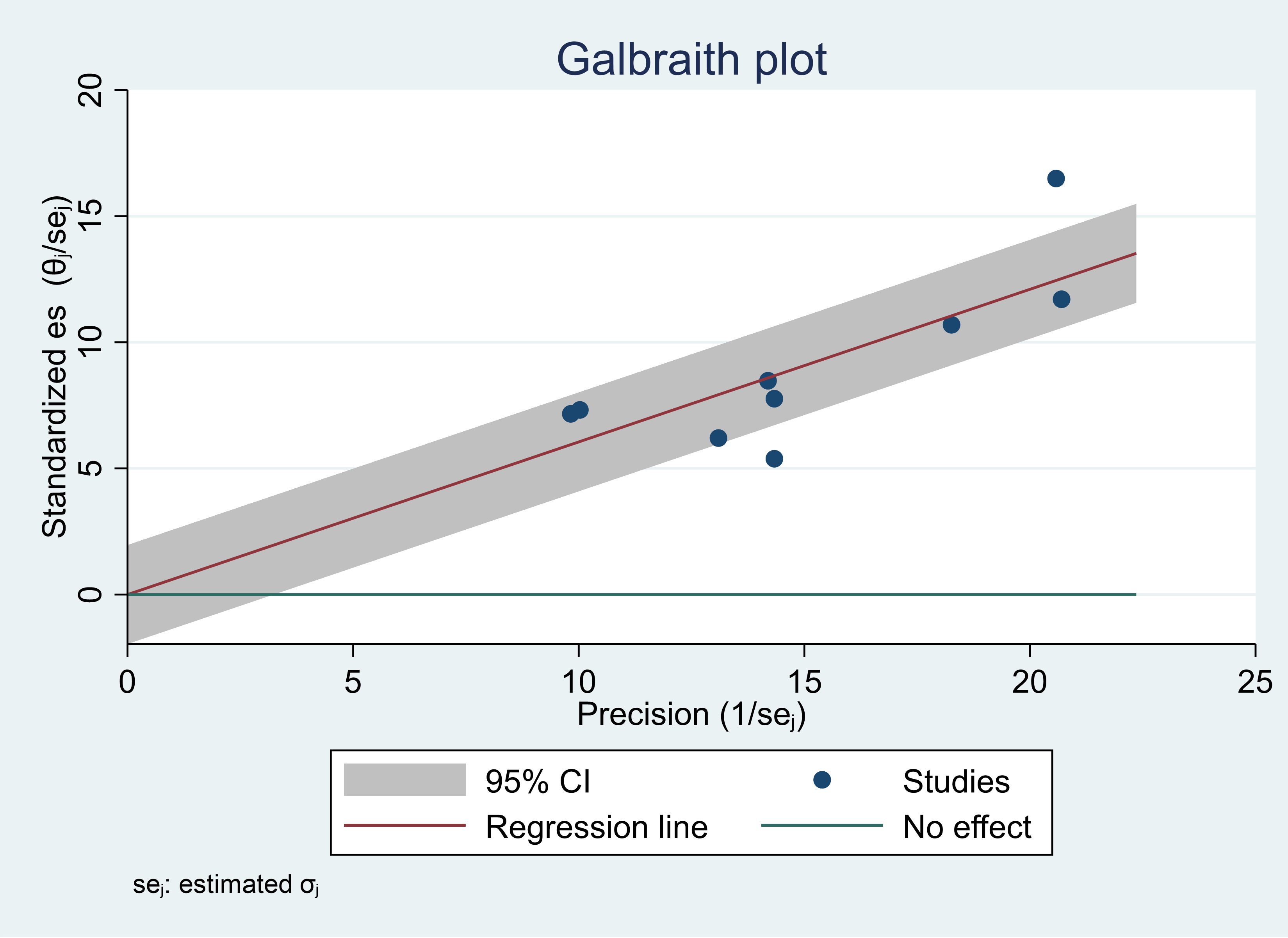
Figure 3. Galbraith plot showing heterogeneity among included studies for the prevalence of depression among breast cancer patients in Sub-Saharan Africa
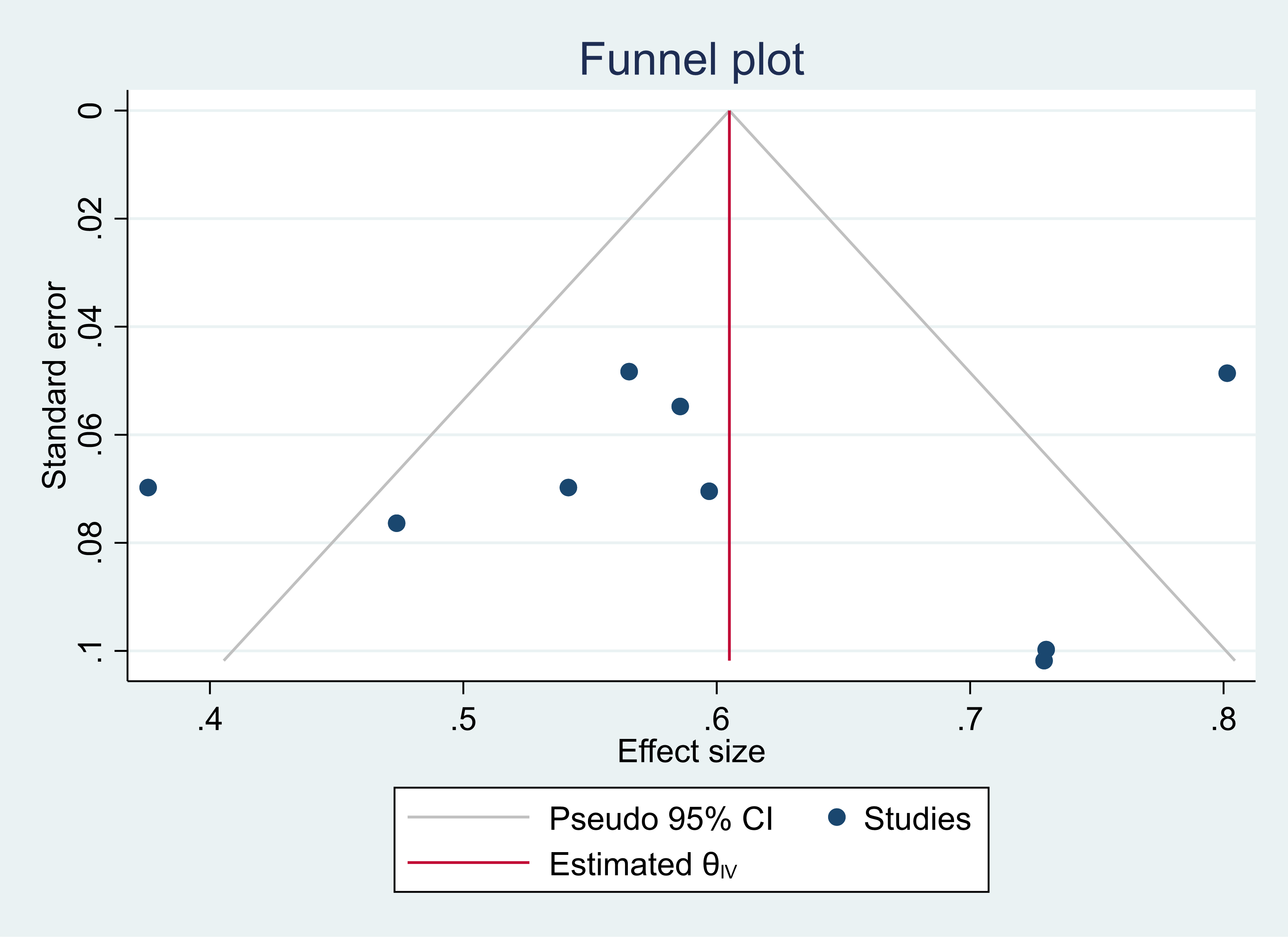
Figure 4. Funnel plot showing the absence of potential publication bias
Leave one out sensitivity analysis
The leave-one-out sensitivity analysis was performed to re-estimate the pooled prevalence of depression, dropping one study at a time. The results revealed that no single study had a significant impact on the overall result.
Sub-group analysis based on regions of Sub-Saharan Africa
Breast cancer patients in East Africa were reported to have a prevalence of depression of 64% (95CI, 0.51-0.75); South Africa reported a prevalence of 60% (95CI, 0.53-0.67); and West Africa reported a prevalence of 55% (95CI, 0.36-0.73). (Figure 6).
The leave-one-out sensitivity analysis was performed to re-estimate the pooled prevalence of depression, dropping one study at a time. The results revealed that no single study had a significant impact on the overall result.
Sub-group analysis based on regions of Sub-Saharan Africa
Breast cancer patients in East Africa were reported to have a prevalence of depression of 64% (95CI, 0.51-0.75); South Africa reported a prevalence of 60% (95CI, 0.53-0.67); and West Africa reported a prevalence of 55% (95CI, 0.36-0.73). (Figure 6).
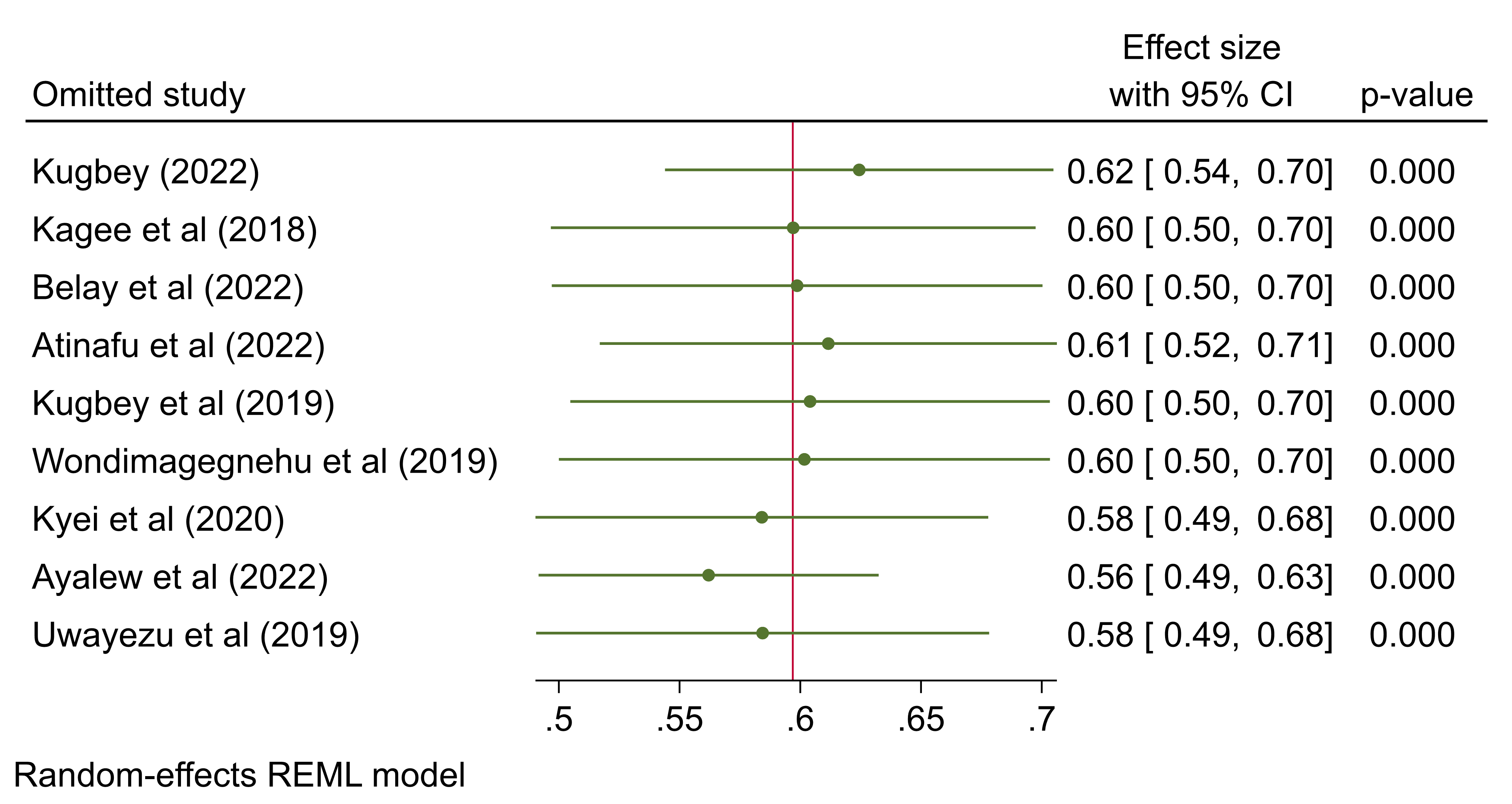
Figure 5. Forest plot showing leave one out sensitivity analysis
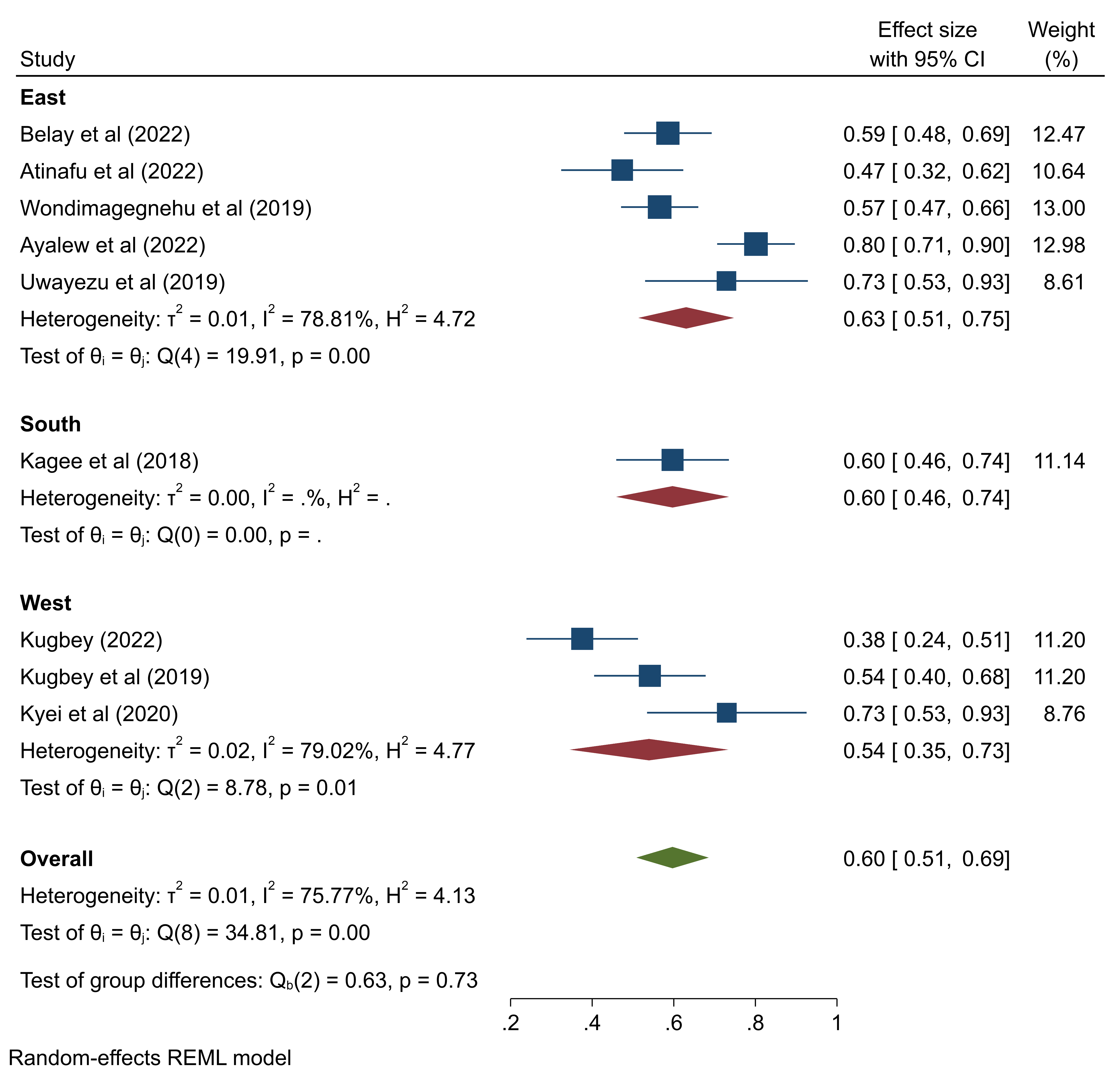
Figure 6. Forest plot showing the pooled prevalence of depression among breast cancer patients in Sub-Saharan Africa by region
Discussion
The current systematic review and meta-analysis aimed to determine the depression prevalence among breast cancer patients in Sub-Saharan Africa. In line with the studies reporting ranges of 9.3%-56%, in the present research, depression affected 60% of cancer patients [6,7]. The prevalence rates of depression were reported as 64%,60%, and 55% among women with breast cancer diagnoses in East Africa, South Africa, and West Africa, respectively. Such a distinction was also noted in studies carried out in Iran and Asian nations [24,25]. Nevertheless, the prevalence of depression varied from 12.5%-31% in cancer patients in Asian countries [26], which is lower than the rates observed in Sub-Saharan Africa. A similar review also reported a prevalence rate of 32.2% [1], which is lower than the rates observed in our study. This variation may be explained by such factors as social support, educational attainment, financial stability, employment status, physical changes, patient-physician relationships, and healthcare systems. Nonetheless, the findings of this study reported an alarming prevalence that requires immediate attention.
Limitations of the study
Among the notable limitations of this study, we can refer to publication bias. Moreover, the study was conducted across several Sub-Saharan African countries; therefore, cultural differences might have affected the prevalence of depression. Furthermore, only one article was extracted from Southern Africa, which may not represent the region.
Conclusions
In Sub-Saharan Africa, about 6 in 10 cancer patients experience depression. Given that The quality of life is negatively impacted by depression, efforts should be made to correctly diagnose depression in order to treat it effectively and efficiently with the fewest possible side effects.
Compliance with ethical guidelines
Not Applicable.
Acknowledgments
Not Applicable.
Authorsʼ contributions
All authors participated in drafting of the article and approved the final version.
Funding/Support
Not Applicable. No support in the form of grants is related to this publication.
Conflicts of Interest
The authors have no conflict of interest to declare in this work.
References
1. Pilevarzadeh M, Amirshahi M, Afsargharehbagh R, Rafiemanesh H, Hashemi SM, Balouchi A. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Research and Treatment. 2019; 176(3):519–33. [DOI: 10.1007/s10549-019-05271-3] [PMID]
2. Hajikarimbaba M, Panahi R, Dehghankar L. Associated factors with adopting preventive behaviors for breast cancer in Iran. Archives of Breast Cancer. 2020; 7(1):37–43. [DOI: 10.32768/abc.20207137-43]
3. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA: A Cancer Journal for Clinicians. 2019; 69(1):7–34. [DOI: 10.3322/caac.21551] [PMID]
4. Khazaei Z, Jarrahi AM, Momenabadi V, Ghorat F, Adineh HA, Sohrabivafa M, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide stomach cancers and their relationship with the human development index (HDI). World Cancer Res J. 2019; 6(9):e1257. [DOI: 10.32113/wcrj_20194_1257]
5. Chlebowski RT, Anderson GL, Aragaki AK, Manson JE, Stefanick ML, Pan K, et al. Association of menopausal hormone therapy with breast cancer incidence and mortality during long-term follow-up of the women's health initiative randomized clinical trials. JAMA. 2020; 324(4):369–80. [DOI: 10.1001/jama.2020.9482] [PMID] [PMCID]
6. Walker J, Hansen CH, Martin P, Symeonides S, Ramessur R, Murray G, et al. Prevalence, associations, and adequacy of treatment of major depression in patients with cancer: a cross-sectional analysis of routinely collected clinical data. The Lancet Psychiatry. 2014; 1(5):343–50. [DOI: 10.1016/S2215-0366(14)70313-X] [PMID]
7. Nikbakhsh N, Moudi S, Abbasian S, Khafri S. Prevalence of depression and anxiety among cancer patients. Caspian Journal of Internal Medicine. 2014; 5(3):167-70. [PMID] [PMCID]
8. Zhu G, Li J, Li J, Wang X, Dai M, Chen J. Depression and survival of breast cancer patients: A protocol for systematic review and meta-analysis. Medicine. 2020; 99(48):e23399. [DOI: 10.1097/MD.0000000000023399] [PMID] [PMCID]
9. McFarland DC, Shaffer KM, Tiersten A, Holland J. Physical symptom burden and its association with distress, anxiety, and depression in breast cancer. Psychosomatics. 2018; 59(5):464–71. [DOI: 10.1016/j.psym.2018.01.005] [PMID] [PMCID]
10. Purkayastha D, Venkateswaran C, Nayar K, Unnikrishnan UG. Prevalence of depression in breast cancer patients and its association with their quality of life: A cross-sectional observational study. Indian Journal of Palliative Care. 2017; 23(3):268-73. [DOI: 10.4103/IJPC.IJPC_6_17] [PMID] [PMCID]
11. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine. 2009; 151(4):264–9. [DOI: 10.7326/0003-4819-151-4-200908180-00135] [PMID]
12. von Hippel PT. The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Medical Research Method-ology. 2015; 15(1):35. [DOI: 10.1186/s12874-015-0024-z] [PMID]
13. Granholm A, Alhazzani W, Møller MH. Use of the GRADE approach in systematic reviews and guidelines. British Journal of Anaesthesia. 2019; 123(5):554–9. [DOI: 10.1016/j.bja.2019.08.015] [PMID]
14. Kugbey N. Comorbid anxiety and depression among women receiving care for breast cancer: analysis of prevalence and associated factors. African Health Sciences. 2022; 22(3):166–72. [DOI: 10.4314/ahs.v22i3.19] [PMID]
15. Swinny CA, Kagee A, Roomaney R. Delayed help-seeking for symptomatic breast cancer: reasons for delay among participants receiving treatment at a public healthcare facility in South Africa. South African Journal of Psychology. 2022; 52(1):87–98. [DOI: 10.1177/0081246321992477]
16. Belay W, Kaba M, Labisso WL, Tigeneh W, Sahile Z, Zergaw A, et al. The effect of interpersonal psychotherapy on quality of life among breast cancer patients with common mental health disorder: a randomized control trial at Tikur Anbessa Specialized Hospital. Supportive Care in Cancer. 2022; 30(1):965–72. [DOI: 10.1007/s00520-021-06508-y]
17. Atinafu BT, Demlew TM, Tarekegn FN. Magnitude of anxiety and depression and associated factors among palliative care patients with cancer at Tikur Anbessa Specialized Hospital, Ethiopia. Ethiopian Journal of Health Sciences. 2022; 32(2):331-42. [DOI: 10.4314/ejhs.v32i2.14] [PMID] [PMCID]
18. Kugbey N, Meyer-Weitz A, Oppong Asante K. Access to health information, health literacy and health-related quality of life among women living with breast cancer: Depression and anxiety as mediators. Patient Education and Counseling. 2019; 102(7):1357–63. [DOI: 10.1016/j.pec.2019.02.014] [PMID]
19. Wondimagegnehu A, Abebe W, Abraha A, Teferra S. Depression and social support among breast cancer patients in Addis Ababa, Ethiopia. BMC cancer. 2019; 19(1):1–8. [DOI: 10.1186/s12885-019-6007-4] [PMID] [PMCID]
20. Kyei KA, Oswald JW, Njoku AU, Kyei JB, Vanderpuye V. Anxiety and depression among breast cancer patients undergoing treatment in Ghana. African Journal of Biomedical Research. 2020; 23(2):227–32.
21. Ayalew M, Deribe B, Duko B, Geleta D, Bogale N, Gemechu L, et al. Prevalence of depression and anxiety symptoms and their determinant factors among patients with cancer in southern Ethiopia: a cross-sectional study. BMJ Open. 2022; 12(1):e051317. [DOI: 10.1136/bmjopen-2021-051317]
22. Uwayezu MG, Gishoma D, Sego R, Mukeshimana M, Collins A. Anxiety and depression among cancer patients: prevalence and associated factors at a Rwandan referral hospital. Rwanda Journal of Medicine and Health Sciences. 2019; 2(2):118–25. [DOI: 10.4314/rjmhs.v2i2.7]
23. Higgins JPT. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. International Journal of Epidemiology. 2008; 37(5):1158–60. [DOI: 10.1093/ije/dyn204] [PMID]
24. Rezaianzadeh A, Mousave M, Hassanipour S, Maghsoudi A, Mokhtari AM, Dehghani SL. Prevalence of depression among iranian women with breast cancer: A Systematic Review and Meta-Analysis. Health Scope. 2019; 8(2):e62781. [DOI: 10.5812/jhealthscope.62781]
25. Ghoncheh M, Mohammadian-Hafshejani A, Salehiniya H. Incidence and mortality of breast cancer and their relationship to development in Asia. Asian Pacific Journal of Cancer Prevention. 2015; 16(14):6081–7. [DOI: 10.7314/apjcp.2015.16.14.6081] [PMID]
26. Zainal NZ, Nik-Jaafar NR, Baharudin A, Sabki ZA, Ng CG. Prevalence of depression in breast cancer survivors: a systematic review of observational studies. Asian Pacific Journal of Cancer Prevention. 2013; 14(4):2649–56. [DOI: 10.7314/apjcp.2013.14.4.2649] [PMID]
The current systematic review and meta-analysis aimed to determine the depression prevalence among breast cancer patients in Sub-Saharan Africa. In line with the studies reporting ranges of 9.3%-56%, in the present research, depression affected 60% of cancer patients [6,7]. The prevalence rates of depression were reported as 64%,60%, and 55% among women with breast cancer diagnoses in East Africa, South Africa, and West Africa, respectively. Such a distinction was also noted in studies carried out in Iran and Asian nations [24,25]. Nevertheless, the prevalence of depression varied from 12.5%-31% in cancer patients in Asian countries [26], which is lower than the rates observed in Sub-Saharan Africa. A similar review also reported a prevalence rate of 32.2% [1], which is lower than the rates observed in our study. This variation may be explained by such factors as social support, educational attainment, financial stability, employment status, physical changes, patient-physician relationships, and healthcare systems. Nonetheless, the findings of this study reported an alarming prevalence that requires immediate attention.
Limitations of the study
Among the notable limitations of this study, we can refer to publication bias. Moreover, the study was conducted across several Sub-Saharan African countries; therefore, cultural differences might have affected the prevalence of depression. Furthermore, only one article was extracted from Southern Africa, which may not represent the region.
Conclusions
In Sub-Saharan Africa, about 6 in 10 cancer patients experience depression. Given that The quality of life is negatively impacted by depression, efforts should be made to correctly diagnose depression in order to treat it effectively and efficiently with the fewest possible side effects.
Compliance with ethical guidelines
Not Applicable.
Acknowledgments
Not Applicable.
Authorsʼ contributions
All authors participated in drafting of the article and approved the final version.
Funding/Support
Not Applicable. No support in the form of grants is related to this publication.
Conflicts of Interest
The authors have no conflict of interest to declare in this work.
References
1. Pilevarzadeh M, Amirshahi M, Afsargharehbagh R, Rafiemanesh H, Hashemi SM, Balouchi A. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Research and Treatment. 2019; 176(3):519–33. [DOI: 10.1007/s10549-019-05271-3] [PMID]
2. Hajikarimbaba M, Panahi R, Dehghankar L. Associated factors with adopting preventive behaviors for breast cancer in Iran. Archives of Breast Cancer. 2020; 7(1):37–43. [DOI: 10.32768/abc.20207137-43]
3. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA: A Cancer Journal for Clinicians. 2019; 69(1):7–34. [DOI: 10.3322/caac.21551] [PMID]
4. Khazaei Z, Jarrahi AM, Momenabadi V, Ghorat F, Adineh HA, Sohrabivafa M, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide stomach cancers and their relationship with the human development index (HDI). World Cancer Res J. 2019; 6(9):e1257. [DOI: 10.32113/wcrj_20194_1257]
5. Chlebowski RT, Anderson GL, Aragaki AK, Manson JE, Stefanick ML, Pan K, et al. Association of menopausal hormone therapy with breast cancer incidence and mortality during long-term follow-up of the women's health initiative randomized clinical trials. JAMA. 2020; 324(4):369–80. [DOI: 10.1001/jama.2020.9482] [PMID] [PMCID]
6. Walker J, Hansen CH, Martin P, Symeonides S, Ramessur R, Murray G, et al. Prevalence, associations, and adequacy of treatment of major depression in patients with cancer: a cross-sectional analysis of routinely collected clinical data. The Lancet Psychiatry. 2014; 1(5):343–50. [DOI: 10.1016/S2215-0366(14)70313-X] [PMID]
7. Nikbakhsh N, Moudi S, Abbasian S, Khafri S. Prevalence of depression and anxiety among cancer patients. Caspian Journal of Internal Medicine. 2014; 5(3):167-70. [PMID] [PMCID]
8. Zhu G, Li J, Li J, Wang X, Dai M, Chen J. Depression and survival of breast cancer patients: A protocol for systematic review and meta-analysis. Medicine. 2020; 99(48):e23399. [DOI: 10.1097/MD.0000000000023399] [PMID] [PMCID]
9. McFarland DC, Shaffer KM, Tiersten A, Holland J. Physical symptom burden and its association with distress, anxiety, and depression in breast cancer. Psychosomatics. 2018; 59(5):464–71. [DOI: 10.1016/j.psym.2018.01.005] [PMID] [PMCID]
10. Purkayastha D, Venkateswaran C, Nayar K, Unnikrishnan UG. Prevalence of depression in breast cancer patients and its association with their quality of life: A cross-sectional observational study. Indian Journal of Palliative Care. 2017; 23(3):268-73. [DOI: 10.4103/IJPC.IJPC_6_17] [PMID] [PMCID]
11. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine. 2009; 151(4):264–9. [DOI: 10.7326/0003-4819-151-4-200908180-00135] [PMID]
12. von Hippel PT. The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Medical Research Method-ology. 2015; 15(1):35. [DOI: 10.1186/s12874-015-0024-z] [PMID]
13. Granholm A, Alhazzani W, Møller MH. Use of the GRADE approach in systematic reviews and guidelines. British Journal of Anaesthesia. 2019; 123(5):554–9. [DOI: 10.1016/j.bja.2019.08.015] [PMID]
14. Kugbey N. Comorbid anxiety and depression among women receiving care for breast cancer: analysis of prevalence and associated factors. African Health Sciences. 2022; 22(3):166–72. [DOI: 10.4314/ahs.v22i3.19] [PMID]
15. Swinny CA, Kagee A, Roomaney R. Delayed help-seeking for symptomatic breast cancer: reasons for delay among participants receiving treatment at a public healthcare facility in South Africa. South African Journal of Psychology. 2022; 52(1):87–98. [DOI: 10.1177/0081246321992477]
16. Belay W, Kaba M, Labisso WL, Tigeneh W, Sahile Z, Zergaw A, et al. The effect of interpersonal psychotherapy on quality of life among breast cancer patients with common mental health disorder: a randomized control trial at Tikur Anbessa Specialized Hospital. Supportive Care in Cancer. 2022; 30(1):965–72. [DOI: 10.1007/s00520-021-06508-y]
17. Atinafu BT, Demlew TM, Tarekegn FN. Magnitude of anxiety and depression and associated factors among palliative care patients with cancer at Tikur Anbessa Specialized Hospital, Ethiopia. Ethiopian Journal of Health Sciences. 2022; 32(2):331-42. [DOI: 10.4314/ejhs.v32i2.14] [PMID] [PMCID]
18. Kugbey N, Meyer-Weitz A, Oppong Asante K. Access to health information, health literacy and health-related quality of life among women living with breast cancer: Depression and anxiety as mediators. Patient Education and Counseling. 2019; 102(7):1357–63. [DOI: 10.1016/j.pec.2019.02.014] [PMID]
19. Wondimagegnehu A, Abebe W, Abraha A, Teferra S. Depression and social support among breast cancer patients in Addis Ababa, Ethiopia. BMC cancer. 2019; 19(1):1–8. [DOI: 10.1186/s12885-019-6007-4] [PMID] [PMCID]
20. Kyei KA, Oswald JW, Njoku AU, Kyei JB, Vanderpuye V. Anxiety and depression among breast cancer patients undergoing treatment in Ghana. African Journal of Biomedical Research. 2020; 23(2):227–32.
21. Ayalew M, Deribe B, Duko B, Geleta D, Bogale N, Gemechu L, et al. Prevalence of depression and anxiety symptoms and their determinant factors among patients with cancer in southern Ethiopia: a cross-sectional study. BMJ Open. 2022; 12(1):e051317. [DOI: 10.1136/bmjopen-2021-051317]
22. Uwayezu MG, Gishoma D, Sego R, Mukeshimana M, Collins A. Anxiety and depression among cancer patients: prevalence and associated factors at a Rwandan referral hospital. Rwanda Journal of Medicine and Health Sciences. 2019; 2(2):118–25. [DOI: 10.4314/rjmhs.v2i2.7]
23. Higgins JPT. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. International Journal of Epidemiology. 2008; 37(5):1158–60. [DOI: 10.1093/ije/dyn204] [PMID]
24. Rezaianzadeh A, Mousave M, Hassanipour S, Maghsoudi A, Mokhtari AM, Dehghani SL. Prevalence of depression among iranian women with breast cancer: A Systematic Review and Meta-Analysis. Health Scope. 2019; 8(2):e62781. [DOI: 10.5812/jhealthscope.62781]
25. Ghoncheh M, Mohammadian-Hafshejani A, Salehiniya H. Incidence and mortality of breast cancer and their relationship to development in Asia. Asian Pacific Journal of Cancer Prevention. 2015; 16(14):6081–7. [DOI: 10.7314/apjcp.2015.16.14.6081] [PMID]
26. Zainal NZ, Nik-Jaafar NR, Baharudin A, Sabki ZA, Ng CG. Prevalence of depression in breast cancer survivors: a systematic review of observational studies. Asian Pacific Journal of Cancer Prevention. 2013; 14(4):2649–56. [DOI: 10.7314/apjcp.2013.14.4.2649] [PMID]
Article Type: Systematic Review or Meta Analysis |
Subject:
Depression
Received: 2023/03/8 | Accepted: 2023/06/18 | Published: 2023/06/30
Received: 2023/03/8 | Accepted: 2023/06/18 | Published: 2023/06/30
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







