Volume 6, Issue 1 (Februrary 2019)
Avicenna J Neuro Psycho Physiology 2019, 6(1): 27-36 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Baghernezhad O, Hasanzadeh R, Abbasi G. Comparing the Effectiveness of Acceptance and Commitment Therapy and Solution-focused Brief Therapy on Pain Catastrophizing and Psychological Well-Being of Patients With Breast Cancer. Avicenna J Neuro Psycho Physiology 2019; 6 (1) :27-36
URL: http://ajnpp.umsha.ac.ir/article-1-151-en.html
URL: http://ajnpp.umsha.ac.ir/article-1-151-en.html
1- Department of Psychology, Islamic Azad University, Sari Branch, Sari, Iran. , bagheri1977@yahoo.com
2- Department of Psychology, Islamic Azad University, Sari Branch, Sari, Iran.
2- Department of Psychology, Islamic Azad University, Sari Branch, Sari, Iran.
Full-Text [PDF 787 kb]
(1363 Downloads)
| Abstract (HTML) (3998 Views)
Full-Text: (1019 Views)
1. Introduction
Cancer is one of the most common diseases in human societies [1]. It causes cells to grow and divide uncontrollably [2]. It is regarded as the third cause of death in Iran after cardiovascular diseases and accidents. Over 30,000 Iranian individuals die from cancer annually. According to some estimates, more than 70,000 new cancer cases are developed in Iran annually. As the second fatal disease among women after lung complaints, breast cancer is a multilateral source of tension, that is, surgery interferences often cause body dysmorphic. Cancer could put the whole mental health in danger; it intensifies one’s stress and threatens mental health mainly because of body dysmorphic [3].
Moreover, the disease causes to create a wide range of psychological problems, such as self-concept and self-esteem threat, losing a feeling of freedom, physical comfort, denial, anger, depression, unreliability, loneliness, and deprivation, as well as family problems. However, studies have consistently shown that those with high psychological well-being offer strong resistance to long-term painful therapies, as well as the effects of chemotherapy and radiation [4]. Generally, the disease, as a strongly stressful event accompanied by difficult and complicated medical processes, causes many psychological problems for the patient and his/her family [5].
On the other hand, catastrophizing is a negative cognitive-emotional process containing exaggeration, distress, and rumination. Catastrophizing level is the main predictor of therapeutic consequences; likewise, it is regarded as a primary variable for cognitive-behavioral approaches and the fear-avoidance model [6]. There is a relationship between catastrophizing and increased sensitivity to pain and emotional disorders; nevertheless, catastrophizing works as an index of disability and harm, when variants such as pain, depression, anxiety, and fear are controlled [7].
Recent evidence suggested that there is a direct link between pain catastrophizing and depression. Unlike men, women show a high-level of pain catastrophizing. Acceptance and Commitment Therapy (ACT) is among non-medicinal psychological therapeutic methods used to harmonize patients with chronic diseases [8]. The approach seeks to help people, but not to pass judgment on what has happened and accept it; it aims at directing them to identify their life values and draw up a good plan [9]. Accepting the fact that a valuable life is always accompanied by distress, commitment is the main ingredient of moving along values, and words could not be displaced by experience will establish fundamental strategies and methods for an acceptance and commitment model [10].
Likewise, Solution-Focused Brief Therapy (SFBT) is one of the most well-known approaches to assist people, who suffer from stress. SFBT has a non-cognitive view of the patient to assist him/her in finding a solution for their current problems [11]. Unlike the problem-oriented approach, it emphasizes finding a solution to the concerned problem. Therefore, the mentioned therapy is based upon solution-making, not problem-solving; it is directed by discovering the current powers of the patient and having hope for the future not discussing current problems and causes thereof [12]. The lack of psychological well-being increases the possibility of patients’ vulnerability to the next problems and happenings. Accordingly, an increase in positive symptoms, rather than negative ones, is the best form of therapy [13].
The ACT has efficient impacts on decreasing depression and pain anxiety. The present research aimed at improving patients’ optimum life conditions by taking into account psychological matters and impacts in appearing or intensifying symptoms of psychosomatic diseases such as cancer [14].
In the same way, notifying the behaviors of medical staff (such as nurses) toward patients to provide them with health services is of the utmost importance. The findings of this study provided valuable information to patients and their families, authorities, specialists, and others to make an effort toward patients’ well-being. The aim of the present research was to compare the effectiveness of ACT with SFBT on the pain catastrophizing and psychological well-being of women with breast cancer.
2. Materials and Methods
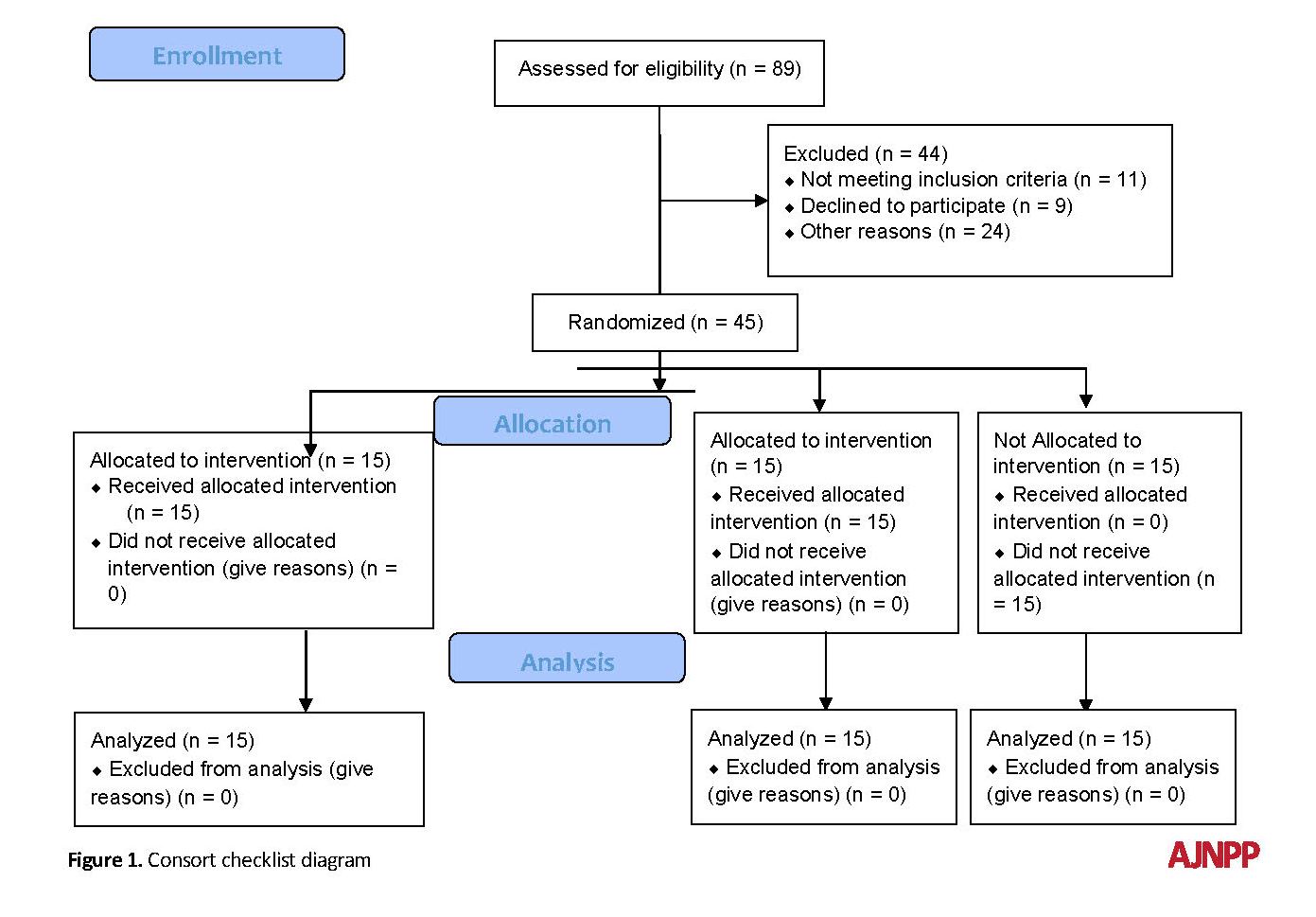
The present quasi-experimental study used a pretest-Post-test design with the control group. The population-based sample consisted of all patients with breast cancer, who were admitted to hospitals and medical centers of Babol and Babolsar in 2018. In order to select the sample, first, a formal announcement was made, stating that the hospital and other private centers would hold medical and training courses. Then, a simple random sample of 45 patients was selected and randomly divided into 3 groups of 15 patients (ACT, SFBT, and control groups).
The criteria of cognition and screening, catastrophizing, and psychological well-being scores were <30 and >50, respectively. Based on the effect size of 0.25, alpha of 0.05, and power of 0.80 in the two groups, the minimum number of samples was determined to achieve the desired power of 15 in each group and 45 in total. Finally, the two experimental groups were subjected to other types of interferences. The inclusion criteria included women with breast cancer based on their medical history, previous experiments, and approval of the disease by the physician, at least a high school degree, and consent to participate in the study. The exclusion criteria included having the history of taking psychological medicine, receiving psychological therapies within the last 6 months, being absent in healing sessions more than twice, having increasingly severe symptoms, and showing function disorder. The patients were randomly divided into the experimental and control groups.
Pain Catastrophizing Scale
Sullivan et al. [15] developed a pain catastrophizing scale in order to evaluate people’s catastrophizing thoughts and behaviors. The self- made questionnaire consisted of 13 variables and needed at least 6 educational levels to reply to questions thereof. The aim of this scale is to study the different aspects of pain catastrophizing and helps patients to understand the effects of the mechanism clearly. It includes 3 sub-scales of rumination, magnificence, and distress. They all evaluate the link between negative thoughts and related pain. The participants are asked to score 13 different thoughts and feelings related to pain experience on a scale of 0 (never) to 4 (always). Questions 8, 9, 10, and 11 considered the rumination on a scale of 0 to 16, questions 6, 7, and 13 were related to magnificence on a scale of 0 to 12, and questions 1, 2, 3, 4, 5, and 12 regarded distress on a scale of 0 to 24. The total pain catastrophizing score was on a scale of 0 to 52. The more the scores, the more catastrophizing the pain. Considering the Cronbach’s alpha, the validity of the other subscales was 0.88, 0.67, and 0.89 for rumination, distress, and magnificence, respectively. To attain the considered power, at least 15 in each group and 45 in total were needed in terms of the effect size (0.25), Cronbach’s alpha (0.05), and power (0.80) [15]. The Iranian version of this scale is a valid and reliable instrument for measuring pain catastrophizing in Iran. Cronbach’s alpha score of reliability was 0.93. Known-groups comparison showed that the pain catastrophizing scale could differentiate between males and females [16].
Psychological Well-being Questionnaire
Psychological well-being is a multi-variant concept containing self-acceptance, good relationships, autonomy, control over the milieu, purposeful life, and personal growth. The questionnaire was designed for adults on a 6-point Likert scale ranging from 1 (completely disagree) to 6 (completely agree), and a form consisting of 18 questions was used therein. To obtain the total score, scores of all questions were summed up. In addition, the total psychological well-being score was calculated by summing up the scores of all 18 questions. By and large, the more the scores, the more the psychological well-being. The correlation of the Ryff’s short psychological well-being scale ranged from 0.7-0.89 [17]. The Iranian version of this scale is a valid and reliable instrument for measuring psychological well-being questionnaire in Iran. Cronbach’s alpha score of Iranian version reliability was 0.79 [18].
Cancer is one of the most common diseases in human societies [1]. It causes cells to grow and divide uncontrollably [2]. It is regarded as the third cause of death in Iran after cardiovascular diseases and accidents. Over 30,000 Iranian individuals die from cancer annually. According to some estimates, more than 70,000 new cancer cases are developed in Iran annually. As the second fatal disease among women after lung complaints, breast cancer is a multilateral source of tension, that is, surgery interferences often cause body dysmorphic. Cancer could put the whole mental health in danger; it intensifies one’s stress and threatens mental health mainly because of body dysmorphic [3].
Moreover, the disease causes to create a wide range of psychological problems, such as self-concept and self-esteem threat, losing a feeling of freedom, physical comfort, denial, anger, depression, unreliability, loneliness, and deprivation, as well as family problems. However, studies have consistently shown that those with high psychological well-being offer strong resistance to long-term painful therapies, as well as the effects of chemotherapy and radiation [4]. Generally, the disease, as a strongly stressful event accompanied by difficult and complicated medical processes, causes many psychological problems for the patient and his/her family [5].
On the other hand, catastrophizing is a negative cognitive-emotional process containing exaggeration, distress, and rumination. Catastrophizing level is the main predictor of therapeutic consequences; likewise, it is regarded as a primary variable for cognitive-behavioral approaches and the fear-avoidance model [6]. There is a relationship between catastrophizing and increased sensitivity to pain and emotional disorders; nevertheless, catastrophizing works as an index of disability and harm, when variants such as pain, depression, anxiety, and fear are controlled [7].
Recent evidence suggested that there is a direct link between pain catastrophizing and depression. Unlike men, women show a high-level of pain catastrophizing. Acceptance and Commitment Therapy (ACT) is among non-medicinal psychological therapeutic methods used to harmonize patients with chronic diseases [8]. The approach seeks to help people, but not to pass judgment on what has happened and accept it; it aims at directing them to identify their life values and draw up a good plan [9]. Accepting the fact that a valuable life is always accompanied by distress, commitment is the main ingredient of moving along values, and words could not be displaced by experience will establish fundamental strategies and methods for an acceptance and commitment model [10].
Likewise, Solution-Focused Brief Therapy (SFBT) is one of the most well-known approaches to assist people, who suffer from stress. SFBT has a non-cognitive view of the patient to assist him/her in finding a solution for their current problems [11]. Unlike the problem-oriented approach, it emphasizes finding a solution to the concerned problem. Therefore, the mentioned therapy is based upon solution-making, not problem-solving; it is directed by discovering the current powers of the patient and having hope for the future not discussing current problems and causes thereof [12]. The lack of psychological well-being increases the possibility of patients’ vulnerability to the next problems and happenings. Accordingly, an increase in positive symptoms, rather than negative ones, is the best form of therapy [13].
The ACT has efficient impacts on decreasing depression and pain anxiety. The present research aimed at improving patients’ optimum life conditions by taking into account psychological matters and impacts in appearing or intensifying symptoms of psychosomatic diseases such as cancer [14].
In the same way, notifying the behaviors of medical staff (such as nurses) toward patients to provide them with health services is of the utmost importance. The findings of this study provided valuable information to patients and their families, authorities, specialists, and others to make an effort toward patients’ well-being. The aim of the present research was to compare the effectiveness of ACT with SFBT on the pain catastrophizing and psychological well-being of women with breast cancer.
2. Materials and Methods
The present quasi-experimental study used a pretest-Post-test design with the control group. The population-based sample consisted of all patients with breast cancer, who were admitted to hospitals and medical centers of Babol and Babolsar in 2018. In order to select the sample, first, a formal announcement was made, stating that the hospital and other private centers would hold medical and training courses. Then, a simple random sample of 45 patients was selected and randomly divided into 3 groups of 15 patients (ACT, SFBT, and control groups).
The criteria of cognition and screening, catastrophizing, and psychological well-being scores were <30 and >50, respectively. Based on the effect size of 0.25, alpha of 0.05, and power of 0.80 in the two groups, the minimum number of samples was determined to achieve the desired power of 15 in each group and 45 in total. Finally, the two experimental groups were subjected to other types of interferences. The inclusion criteria included women with breast cancer based on their medical history, previous experiments, and approval of the disease by the physician, at least a high school degree, and consent to participate in the study. The exclusion criteria included having the history of taking psychological medicine, receiving psychological therapies within the last 6 months, being absent in healing sessions more than twice, having increasingly severe symptoms, and showing function disorder. The patients were randomly divided into the experimental and control groups.
Pain Catastrophizing Scale
Sullivan et al. [15] developed a pain catastrophizing scale in order to evaluate people’s catastrophizing thoughts and behaviors. The self- made questionnaire consisted of 13 variables and needed at least 6 educational levels to reply to questions thereof. The aim of this scale is to study the different aspects of pain catastrophizing and helps patients to understand the effects of the mechanism clearly. It includes 3 sub-scales of rumination, magnificence, and distress. They all evaluate the link between negative thoughts and related pain. The participants are asked to score 13 different thoughts and feelings related to pain experience on a scale of 0 (never) to 4 (always). Questions 8, 9, 10, and 11 considered the rumination on a scale of 0 to 16, questions 6, 7, and 13 were related to magnificence on a scale of 0 to 12, and questions 1, 2, 3, 4, 5, and 12 regarded distress on a scale of 0 to 24. The total pain catastrophizing score was on a scale of 0 to 52. The more the scores, the more catastrophizing the pain. Considering the Cronbach’s alpha, the validity of the other subscales was 0.88, 0.67, and 0.89 for rumination, distress, and magnificence, respectively. To attain the considered power, at least 15 in each group and 45 in total were needed in terms of the effect size (0.25), Cronbach’s alpha (0.05), and power (0.80) [15]. The Iranian version of this scale is a valid and reliable instrument for measuring pain catastrophizing in Iran. Cronbach’s alpha score of reliability was 0.93. Known-groups comparison showed that the pain catastrophizing scale could differentiate between males and females [16].
Psychological Well-being Questionnaire
Psychological well-being is a multi-variant concept containing self-acceptance, good relationships, autonomy, control over the milieu, purposeful life, and personal growth. The questionnaire was designed for adults on a 6-point Likert scale ranging from 1 (completely disagree) to 6 (completely agree), and a form consisting of 18 questions was used therein. To obtain the total score, scores of all questions were summed up. In addition, the total psychological well-being score was calculated by summing up the scores of all 18 questions. By and large, the more the scores, the more the psychological well-being. The correlation of the Ryff’s short psychological well-being scale ranged from 0.7-0.89 [17]. The Iranian version of this scale is a valid and reliable instrument for measuring psychological well-being questionnaire in Iran. Cronbach’s alpha score of Iranian version reliability was 0.79 [18].
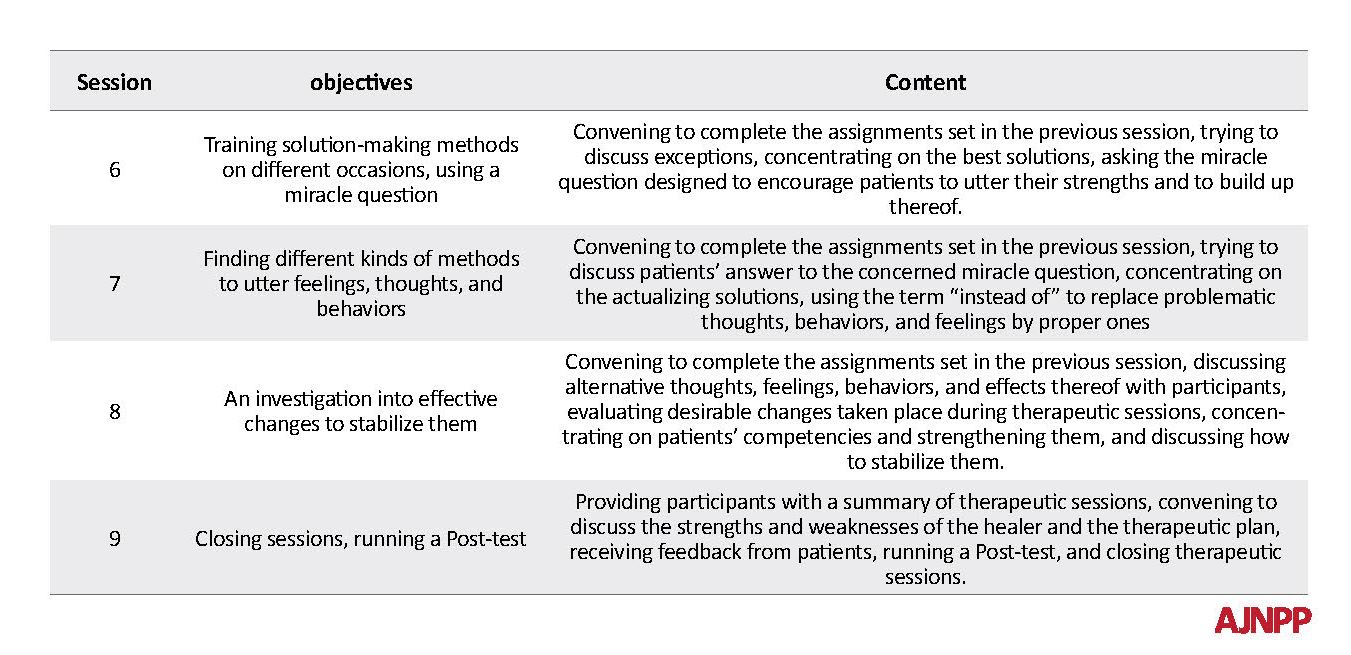
The pretest was run for the two experimental groups; then, the ACT and SFBT groups received 9 sessions of 90-minute interferences for 9 weeks (Table 1 & 2). But, no interference was applied to the control group. Next, the Post-test was run for the control and experimental groups. The participants were free to cooperate in or leave the survey whenever they wish. The researcher explained scientific reasoning for the participants. They were ensured that any information given during the interview would be confidential. It was essential to establish that their intellectual property would be preserved when the results of the research would be published. The participants attended the experiment entirely for free.
The second group received SFBT. The researcher held 9 sessions of 90-minute SFBT (once a week for 6 weeks) to examine the variables of the experimental groups. The descriptive statistics (Mean±SD) and inferential statistics were used to analyze the data by SPSS 23.
3. Results
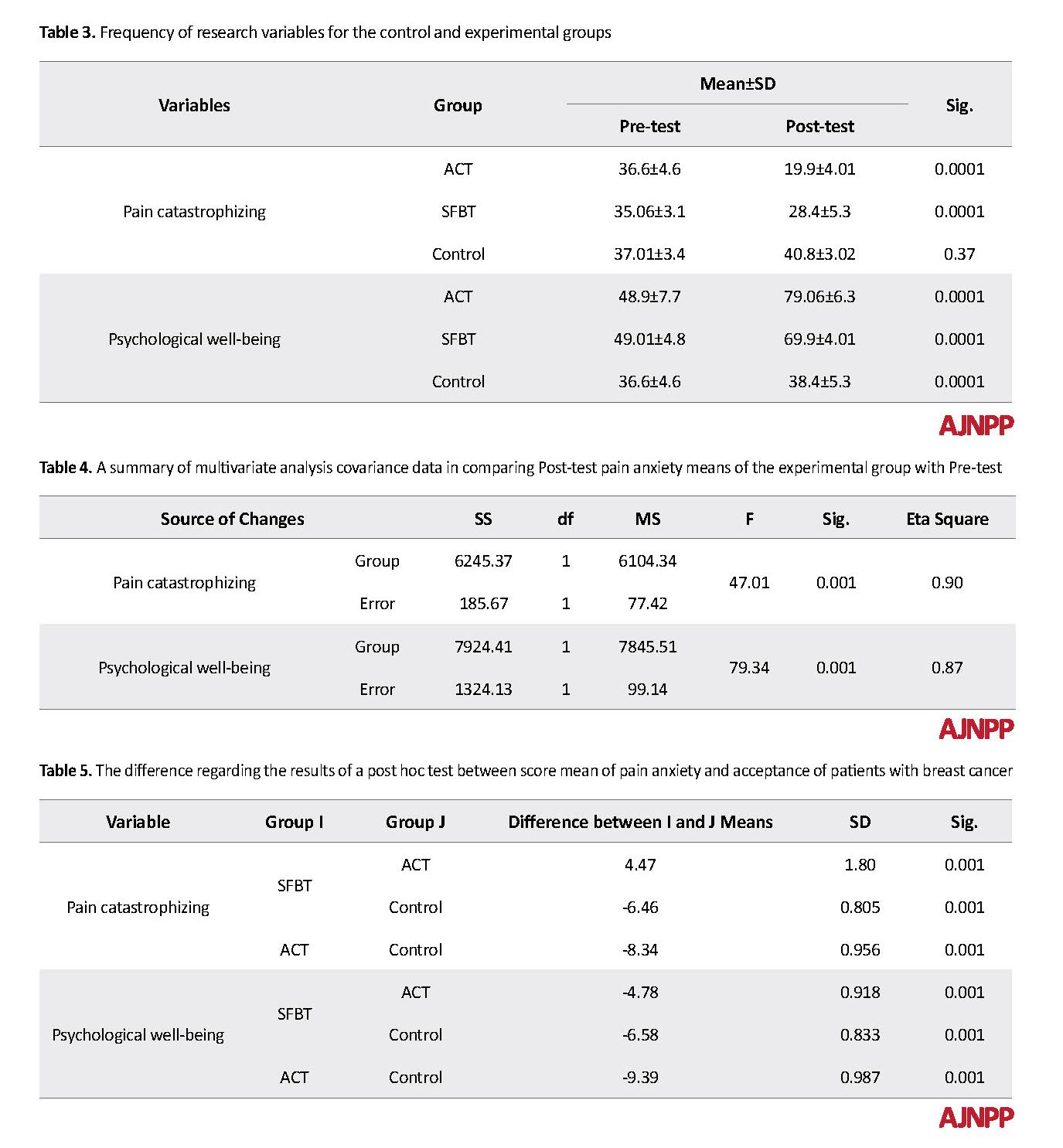
The Mean±SD age of participants in the ACT, SFBT, and control groups were 36.2 ± 7.4, 35.7 ± 7.2, and 38.1 ± 9.4 years, respectively, which ranged from 20 to 60 years. In terms of education, 18 (30%), 24 (40%), and 18 (30%) patients had a diploma, bachelors’ degree, and master’s degree, respectively (Table 3).
Before running the multivariate analysis covariance test, both Box and Levene’s tests were administered to consider their assumptions. Based on the Box test, it was not significant for any variables. The homogeneity assumption of variance/covariance was observed, as well. Based on the Wilks’ lambda criterion, which was not significant for all variables, the evenness condition has been considered for all groups. Therefore, it was allowed to use a variance analysis test (Table 4).
The F value was significant for the experimental groups, pain catastrophizing, and psychological well-being (P>0.01). One of the mentioned therapies at least had to impact on pain catastrophizing and psychological well-being in women with breast cancer (Table 5).
3. Results
The Mean±SD age of participants in the ACT, SFBT, and control groups were 36.2 ± 7.4, 35.7 ± 7.2, and 38.1 ± 9.4 years, respectively, which ranged from 20 to 60 years. In terms of education, 18 (30%), 24 (40%), and 18 (30%) patients had a diploma, bachelors’ degree, and master’s degree, respectively (Table 3).
Before running the multivariate analysis covariance test, both Box and Levene’s tests were administered to consider their assumptions. Based on the Box test, it was not significant for any variables. The homogeneity assumption of variance/covariance was observed, as well. Based on the Wilks’ lambda criterion, which was not significant for all variables, the evenness condition has been considered for all groups. Therefore, it was allowed to use a variance analysis test (Table 4).
The F value was significant for the experimental groups, pain catastrophizing, and psychological well-being (P>0.01). One of the mentioned therapies at least had to impact on pain catastrophizing and psychological well-being in women with breast cancer (Table 5).
According to Table 5, although both medical practices suggested a profound effect on catastrophic pain and psychological well-being on patients with breast cancer, the impact of the ACT was more significant (P>0.01).
4. Discussion
The present research aimed at comparing the impact of ACT with SFBT on pain catastrophizing and psychological well-being among women with breast cancer. However, both variables represented no significant difference for the pretest and Post-test in the control group.
The findings of the current study were consistent with those of Hann and McCracken [19] and Arch et al. [20], who studied the effectiveness of ACT in chronic pain and anxiety disorders, respectively. However, to date, there was no consensus about the impact of SFBT on pain catastrophizing and psychological well-being. In conclusion, there was a close link between the acceptance of pain and more involvement in routine activities.
Likewise, these results suggested a strong relationship between acceptance and cognitive control. In the same way, researchers concluded that pain acceptance was among the most well-known practice to remove undesirable life aspects [21]. Several studies confirmed that the acceptance of pain plays a pivotal role in the daily functions of people with chronic pains. Based on the clinical studies, although there was a weak relationship between pain acceptance and pain experience of psychological and physical problems, a close link exists between pain acceptance and psychological well-being [22].
Recent studies showed a definite link among pain acceptance with high quality of life among patients with backache [23], the decrease in the impact of pain periods on the function of patients with rheumatoid arthritis [24], as well as the improvements in the function of patients with various pains [25].
The ACT is among the most effective acceptance-based inferences for those intending to experience undesirable psychological events such as pain. Acceptance-based inferences cause low sensitivity to chronic pains. The ACT is regarded as an approach subset indicating that acceptance has a leading role in decreasing the pain experience among patients with chronic pains. The acceptance seems to be an essential process involved in medicinal achievements, which increases painful functions and predicates future one’s functions. Turner et al. [26] have shown that unlike other medicinal practices, the therapy has a profound impact on decreasing pain catastrophizing experience among patients. Pain catastrophizing is a warning for chronic pain and disability.
Moreover, some researchers have studied the assumption that the pain gets worse mainly because of the impact of pain catastrophizing on attention processes. In other words, high catastrophizing level leads to intense selective attention to driving-related pain [27]. Unlike non-catastrophic experience, catastrophic experience has more trouble to control or relieve pain-relevant thoughts. They usually ruminate over pain; so, their cognitive and physical functions are more unbalanced through pain expectancy [28].
The ACT causes a significant decrease in pain catastrophizing among patients. Indeed, thinking processes thought participates in leaving supersession convection and helping to release them from disturbing thoughts [29]. The ACT has a leading impact on decreasing the pain catastrophizing among patients with breast cancer. Moreover, compared to SFBT, ACT showed a leading effect on pain catastrophizing and psychological well-being among patients with breast cancer [30]. It is worth noting that there exists a positive relationship between the mental health of chronic pain-stricken patients and doing daily activities. Also, there exists a definite link between pain acceptance and high quality of life among patients with backache, which has decreased the impact of painful periods in the function of patients with rheumatoid arthritis, as well as improvements in the function of patients with various pains [31].
Likewise, the results revealed the effectiveness of ACT in patients, who suffered from experimental inductive pain. In addition, studies conducted based on the clinical surveys emphasized the importance of ACT for decreased pain symptoms and increased psychological well-being accompanied by pain. The cognitive resilience establishes the main theoretical ingredient in acceptance based on behavioral therapies such as ACT [32]
SFBT is more effective in social emergency and matrimony conflicts. Using trained skills, the participants could be familiarized with their characteristics and sought to correct themselves implying on positive points and displacing them by rational thoughts rather than undesirable cognitive distortions and tried to improve their thoughts and feelings. The skills help the patients reveal their inherent capabilities, using positive compatible behaviors through taking control of their stress by the use of stress-fighting skills. People show incompatible behavior when the current condition threatens their health. Therefore, the improved condition will help people to reveal more cooperative behavior.
The participants were taught how to displace confidence by doubt; they recognized their cognitive distortions through reorganizing their negative thoughts and displaced thereof by proper reasonable thoughts. Regarding the limitations of the present research, imp generalizing the results should be done cautiously. The current study has only examined women with breast cancer in hospitals and health centers of Babol and Babolsar. Therefore, it is essential to be aware of generalizing the results to the patients of other cities. As another limitation of this study, the follow-up study was not conducted mainly because of time restriction and inaccessibility to the participants. There is ample room for further work to establish the function of the studied therapy regarding Iranian culture, using comparing the effectiveness of the ACT accompanied by other medicinal approaches. It is recommended to take a follow-up test at the end of therapy to evaluate long-term effects thereof and establish closing training sessions.
5. Conclusion
Although both ACT and SFBT represented an excellent impact on decreasing the pain catastrophizing and increasing the psychological well-being, the first was more successful.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages and signed the informed consent; they were also assured about the confidentiality of their information. Moreover, they were allowed to leave the study whenever they wish and, if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed equally in preparing all parts of the research.
Conflict of interest
The authors declared no conflict of interest.
References
Pudkasam S, Tangalakis K, Chinlumprasert N, Apostolopoulos V, Stojanovska L. Breast cancer and exercise: The role of adiposity and immune markers. Maturitas. 2017; 105:16-22. [DOI:10.1016/j.maturitas.2017.04.022] [PMID]
Shinden Y, Kijima Y, Hirata M, Nakajo A, Tanoue K, Arigami T, et al. Clinical characteristics of breast cancer patients with mental disorders. Breast. 2017; 36:39-43. [DOI:10.1016/j.breast.2017.08.010] [PMID]
Stephens PJ, Tarpey PS, Davies H, Van Loo P, Greenman C, Wedge DC, et al. The landscape of cancer genes and mutational processes in breast cancer. Nature. 2012; 486(7403):400-15. [DOI:10.1038/nature11017] [PMID] [PMCID]
Sachs N, de Ligt J, Kopper O, Gogola E, Bounova G, Weeber F, et al. A living biobank of breast cancer organoids captures disease heterogeneity. Cell. 2018; 172(1-2):373-86. [DOI:10.1016/j.cell.2017.11.010] [PMID]
Swain SM, Baselga J, Kim SB, Ro J, Semiglazov V, Campone M, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. New England Journal of Medicine. 2015; 372(8):724-34. [DOI:10.1056/NEJMoa1413513] [PMID] [PMCID]
DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA: a cancer journal for clinicians. 2016; 66(1):31-42. [DOI:10.3322/caac.21320] [PMID]
Kale HP, Carroll NV. Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among US cancer survivors. Cancer. 2016; 122(8):283-9. [DOI:10.1002/cncr.29808] [PMID]
Salari Rad Z, Ghorbani N, Bagheri F. Self-Control role in responding to the stress of breast cancer. Rooyesh-e-Ravanshenasi. 2016; 4(4):15-22.
Proserpio T, Ferrari A, Lo Vullo S, Massimino M, Clerici CA, Veneroni L, et al. Hope in cancer patients: The relational domain as a crucial factor. Tumori. 2015; 101(4):447-54. [DOI:10.5301/tj.5000366] [PMID]
Mansano-Schlosser TC, Ceolim MF, Valerio TD. Poor sleep quality, depression and hope before breast cancer surgery. Appl Nurs Res. 2017; 34:7-11. [DOI:10.1016/j.apnr.2016.11.010] [PMID]
Berendes D, Keefe FJ, Somers TJ, Kothadia SM, Porter LS, Cheavens JS. Hope in the context of lung cancer: Relationships of hope to symptoms and psychological distress. J Pain Symptom Manage. 2010; 40(2):174-82. [DOI:10.1016/j.jpainsymman.2010.01.014] [PMID] [PMCID]
Mousvi Diva R, Moghadam N, Amani O. Evaluating family functioning and spiritual health in women with breast cancer, cancer-treated, and healthy women. J Nurs Educ 2017; 5(5):49-56. [DOI:10.21859/ijpn-05057]
SeyedTabaee R, Rahmatinejad P, Mohammadi D, Etemad A. The role of coping strategies and cognitive emotion regulation in well-being of patients with cancer. J Qazvin Univ Med Sci. 2017; 21(2):41-9.
Reich RR, Lengacher CA, Alinat CB, Kip KE, Paterson C, Ramesar S, et al. Mindfulness-based stress reduction in post-treatment breast cancer patients: Immediate and sustained effects across multiple symptom clusters. Journal of Pain and Symptom Management. 2017; 53(1):85-95. [DOI:10.1016/j.jpainsymman.2016.08.005] [PMID]
Sullivan M J L, Bishop S, Pivik J. The pain catastrophizing scale: Development and validation psychol assess. 1995; 7(4):524-32. [DOI:10.1037/1040-3590.7.4.524]
Raeissadat SA, Sadeghi S, Montazeri A. Validation of the pain catastrophizing scale (PCS) in Iran. J Basic Appl Sci Res. 2013; 3(9):376-80.
Ryff CD, Singer B. The contours of positive human health. Psychol Inq. 1998; 9(1):1-28. [DOI:10.1207/s15327965pli0901_1]
Souri H, Hasanirad T. Relationship between resilience, optimism and psychological well-being in students of medicine. Procedia-Social and Behavioral Sciences. 2011; 30:1541-4. [DOI:10.1016/j.sbspro.2011.10.299]
Hann KE, McCracken LM. A systematic review of randomized controlled trials of Acceptance and Commitment Therapy for adults with chronic pain: Outcome domains, design quality, and efficacy. Journal of Contextual Behavioral Science. 2014; 3(4):217-27. [DOI:10.1016/j.jcbs.2014.10.001]
Arch JJ, Wolitzky-Taylor KB, Eifert GH, Craske MG. Longitudinal treatment mediation of traditional cognitive behavioral therapy and acceptance and commitment therapy for anxiety disorders. Behaviour Research and Therapy. 2012; 50(7-8):469-78. [DOI:10.1016/j.brat.2012.04.007] [PMID]
Åkerblom S, Perrin S, Fischer MR, McCracken LM. The mediating role of acceptance in multidisciplinary cognitive-behavioral therapy for chronic pain. The Journal of Pain. 2015; 16(7):606-15. [DOI:10.1016/j.jpain.2015.03.007] [PMID]
Herbert MS, Afari N, Robinson JB, Listvinsky A, Bondi MW, Wetherell JL. Neuropsychological functioning and treatment outcomes in acceptance and commitment therapy for chronic pain. The Journal of Pain. 2018; 19(8):852-61. [DOI:10.1016/j.jpain.2018.02.008] [PMID]
Scott W, Hann KE, McCracken LM. A comprehensive examination of changes in psychological flexibility following acceptance and commitment therapy for chronic pain. Journal of Contemporary Psychotherapy. 2016; 46(3):139-48. [DOI:10.1007/s10879-016-9328-5] [PMID] [PMCID]
Martel ME, Dionne F, Scott W. The mediating role of pain acceptance in the relation between perceived injustice and chronic pain outcomes in a community sample. The Clinical Journal of Pain. 2017; 33(6):509-16. [DOI:10.1097/AJP.0000000000000427] [PMID]
Clementi MA, Kao GS, Monico E. Pain acceptance as a predictor of medical utilization and school absenteeism in adolescents with chronic pain. Journal of Pediatric Psychology. 2017; 43(3):294-302. [DOI:10.1093/jpepsy/jsx125] [PMID]
Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KM. Acceptance-and mindfulness-based interventions for the treatment of chronic pain: A meta-analytic review. Cognitive Behaviour Therapy. 2016; 45(1):5-31. [DOI:10.1080/16506073.2015.1098724] [PMID]
Turner J, Sherman K, Anderson M, Balderson B, Cook A, Cherkin D. Catastrophizing, pain self-efficacy, mindfulness, and acceptance: Relationships and changes among individuals receiving CBT, MBSR, or usual care for chronic back pain. The Journal of Pain. 2015; 16(4):96-107. [DOI:10.1016/j.jpain.2015.01.401]
Lillis J, Graham Thomas J, Seng EK, Lipton RB, Pavlovi JM, et al. Importance of pain acceptance in relation to headache disability and pain interference in women with migraine and overweight/obesity. Headache: The Journal of Head and Face Pain. 2017; 57(5):709-18. [DOI:10.1111/head.13058] [PMID] [PMCID]
Baranoff JA, Hanrahan SJ, Burke AL, Connor JP. Changes in acceptance in a low-intensity, group-based acceptance and commitment therapy (ACT) chronic pain intervention. International Journal of Behavioral Medicine. 2016; 23(1):30-8. [DOI:10.1007/s12529-015-9496-9] [PMID]
Goubert L, Crombez G, Van Damme S. The role of neuroticism, pain catastrophizing and pain-related fear in vigilance to pain: A structural equations approach. Pain. 2004; 107(3):234-41. [DOI:10.1016/j.pain.2003.11.005] [PMID]
Lin J, Paganini S, Sander L, Lüking M, Ebert DD, Buhrman M, et al. An internet-based intervention for chronic pain: A three-arm randomized controlled study of the effectiveness of guided and unguided acceptance and commitment therapy. Deutsches Ärzteblatt International. 2017; 114(41):681-97.
Simpson PA, Mars T, Esteves JE. A systematic review of randomised controlled trials using Acceptance and commitment therapy as an intervention in the management of non-malignant, chronic pain in adults. International Journal of Osteopathic Medicine. 2017; 24:18-31. [DOI:10.1016/j.ijosm.2017.03.001]
4. Discussion
The present research aimed at comparing the impact of ACT with SFBT on pain catastrophizing and psychological well-being among women with breast cancer. However, both variables represented no significant difference for the pretest and Post-test in the control group.
The findings of the current study were consistent with those of Hann and McCracken [19] and Arch et al. [20], who studied the effectiveness of ACT in chronic pain and anxiety disorders, respectively. However, to date, there was no consensus about the impact of SFBT on pain catastrophizing and psychological well-being. In conclusion, there was a close link between the acceptance of pain and more involvement in routine activities.
Likewise, these results suggested a strong relationship between acceptance and cognitive control. In the same way, researchers concluded that pain acceptance was among the most well-known practice to remove undesirable life aspects [21]. Several studies confirmed that the acceptance of pain plays a pivotal role in the daily functions of people with chronic pains. Based on the clinical studies, although there was a weak relationship between pain acceptance and pain experience of psychological and physical problems, a close link exists between pain acceptance and psychological well-being [22].
Recent studies showed a definite link among pain acceptance with high quality of life among patients with backache [23], the decrease in the impact of pain periods on the function of patients with rheumatoid arthritis [24], as well as the improvements in the function of patients with various pains [25].
The ACT is among the most effective acceptance-based inferences for those intending to experience undesirable psychological events such as pain. Acceptance-based inferences cause low sensitivity to chronic pains. The ACT is regarded as an approach subset indicating that acceptance has a leading role in decreasing the pain experience among patients with chronic pains. The acceptance seems to be an essential process involved in medicinal achievements, which increases painful functions and predicates future one’s functions. Turner et al. [26] have shown that unlike other medicinal practices, the therapy has a profound impact on decreasing pain catastrophizing experience among patients. Pain catastrophizing is a warning for chronic pain and disability.
Moreover, some researchers have studied the assumption that the pain gets worse mainly because of the impact of pain catastrophizing on attention processes. In other words, high catastrophizing level leads to intense selective attention to driving-related pain [27]. Unlike non-catastrophic experience, catastrophic experience has more trouble to control or relieve pain-relevant thoughts. They usually ruminate over pain; so, their cognitive and physical functions are more unbalanced through pain expectancy [28].
The ACT causes a significant decrease in pain catastrophizing among patients. Indeed, thinking processes thought participates in leaving supersession convection and helping to release them from disturbing thoughts [29]. The ACT has a leading impact on decreasing the pain catastrophizing among patients with breast cancer. Moreover, compared to SFBT, ACT showed a leading effect on pain catastrophizing and psychological well-being among patients with breast cancer [30]. It is worth noting that there exists a positive relationship between the mental health of chronic pain-stricken patients and doing daily activities. Also, there exists a definite link between pain acceptance and high quality of life among patients with backache, which has decreased the impact of painful periods in the function of patients with rheumatoid arthritis, as well as improvements in the function of patients with various pains [31].
Likewise, the results revealed the effectiveness of ACT in patients, who suffered from experimental inductive pain. In addition, studies conducted based on the clinical surveys emphasized the importance of ACT for decreased pain symptoms and increased psychological well-being accompanied by pain. The cognitive resilience establishes the main theoretical ingredient in acceptance based on behavioral therapies such as ACT [32]
SFBT is more effective in social emergency and matrimony conflicts. Using trained skills, the participants could be familiarized with their characteristics and sought to correct themselves implying on positive points and displacing them by rational thoughts rather than undesirable cognitive distortions and tried to improve their thoughts and feelings. The skills help the patients reveal their inherent capabilities, using positive compatible behaviors through taking control of their stress by the use of stress-fighting skills. People show incompatible behavior when the current condition threatens their health. Therefore, the improved condition will help people to reveal more cooperative behavior.
The participants were taught how to displace confidence by doubt; they recognized their cognitive distortions through reorganizing their negative thoughts and displaced thereof by proper reasonable thoughts. Regarding the limitations of the present research, imp generalizing the results should be done cautiously. The current study has only examined women with breast cancer in hospitals and health centers of Babol and Babolsar. Therefore, it is essential to be aware of generalizing the results to the patients of other cities. As another limitation of this study, the follow-up study was not conducted mainly because of time restriction and inaccessibility to the participants. There is ample room for further work to establish the function of the studied therapy regarding Iranian culture, using comparing the effectiveness of the ACT accompanied by other medicinal approaches. It is recommended to take a follow-up test at the end of therapy to evaluate long-term effects thereof and establish closing training sessions.
5. Conclusion
Although both ACT and SFBT represented an excellent impact on decreasing the pain catastrophizing and increasing the psychological well-being, the first was more successful.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages and signed the informed consent; they were also assured about the confidentiality of their information. Moreover, they were allowed to leave the study whenever they wish and, if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed equally in preparing all parts of the research.
Conflict of interest
The authors declared no conflict of interest.
References
Pudkasam S, Tangalakis K, Chinlumprasert N, Apostolopoulos V, Stojanovska L. Breast cancer and exercise: The role of adiposity and immune markers. Maturitas. 2017; 105:16-22. [DOI:10.1016/j.maturitas.2017.04.022] [PMID]
Shinden Y, Kijima Y, Hirata M, Nakajo A, Tanoue K, Arigami T, et al. Clinical characteristics of breast cancer patients with mental disorders. Breast. 2017; 36:39-43. [DOI:10.1016/j.breast.2017.08.010] [PMID]
Stephens PJ, Tarpey PS, Davies H, Van Loo P, Greenman C, Wedge DC, et al. The landscape of cancer genes and mutational processes in breast cancer. Nature. 2012; 486(7403):400-15. [DOI:10.1038/nature11017] [PMID] [PMCID]
Sachs N, de Ligt J, Kopper O, Gogola E, Bounova G, Weeber F, et al. A living biobank of breast cancer organoids captures disease heterogeneity. Cell. 2018; 172(1-2):373-86. [DOI:10.1016/j.cell.2017.11.010] [PMID]
Swain SM, Baselga J, Kim SB, Ro J, Semiglazov V, Campone M, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. New England Journal of Medicine. 2015; 372(8):724-34. [DOI:10.1056/NEJMoa1413513] [PMID] [PMCID]
DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA: a cancer journal for clinicians. 2016; 66(1):31-42. [DOI:10.3322/caac.21320] [PMID]
Kale HP, Carroll NV. Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among US cancer survivors. Cancer. 2016; 122(8):283-9. [DOI:10.1002/cncr.29808] [PMID]
Salari Rad Z, Ghorbani N, Bagheri F. Self-Control role in responding to the stress of breast cancer. Rooyesh-e-Ravanshenasi. 2016; 4(4):15-22.
Proserpio T, Ferrari A, Lo Vullo S, Massimino M, Clerici CA, Veneroni L, et al. Hope in cancer patients: The relational domain as a crucial factor. Tumori. 2015; 101(4):447-54. [DOI:10.5301/tj.5000366] [PMID]
Mansano-Schlosser TC, Ceolim MF, Valerio TD. Poor sleep quality, depression and hope before breast cancer surgery. Appl Nurs Res. 2017; 34:7-11. [DOI:10.1016/j.apnr.2016.11.010] [PMID]
Berendes D, Keefe FJ, Somers TJ, Kothadia SM, Porter LS, Cheavens JS. Hope in the context of lung cancer: Relationships of hope to symptoms and psychological distress. J Pain Symptom Manage. 2010; 40(2):174-82. [DOI:10.1016/j.jpainsymman.2010.01.014] [PMID] [PMCID]
Mousvi Diva R, Moghadam N, Amani O. Evaluating family functioning and spiritual health in women with breast cancer, cancer-treated, and healthy women. J Nurs Educ 2017; 5(5):49-56. [DOI:10.21859/ijpn-05057]
SeyedTabaee R, Rahmatinejad P, Mohammadi D, Etemad A. The role of coping strategies and cognitive emotion regulation in well-being of patients with cancer. J Qazvin Univ Med Sci. 2017; 21(2):41-9.
Reich RR, Lengacher CA, Alinat CB, Kip KE, Paterson C, Ramesar S, et al. Mindfulness-based stress reduction in post-treatment breast cancer patients: Immediate and sustained effects across multiple symptom clusters. Journal of Pain and Symptom Management. 2017; 53(1):85-95. [DOI:10.1016/j.jpainsymman.2016.08.005] [PMID]
Sullivan M J L, Bishop S, Pivik J. The pain catastrophizing scale: Development and validation psychol assess. 1995; 7(4):524-32. [DOI:10.1037/1040-3590.7.4.524]
Raeissadat SA, Sadeghi S, Montazeri A. Validation of the pain catastrophizing scale (PCS) in Iran. J Basic Appl Sci Res. 2013; 3(9):376-80.
Ryff CD, Singer B. The contours of positive human health. Psychol Inq. 1998; 9(1):1-28. [DOI:10.1207/s15327965pli0901_1]
Souri H, Hasanirad T. Relationship between resilience, optimism and psychological well-being in students of medicine. Procedia-Social and Behavioral Sciences. 2011; 30:1541-4. [DOI:10.1016/j.sbspro.2011.10.299]
Hann KE, McCracken LM. A systematic review of randomized controlled trials of Acceptance and Commitment Therapy for adults with chronic pain: Outcome domains, design quality, and efficacy. Journal of Contextual Behavioral Science. 2014; 3(4):217-27. [DOI:10.1016/j.jcbs.2014.10.001]
Arch JJ, Wolitzky-Taylor KB, Eifert GH, Craske MG. Longitudinal treatment mediation of traditional cognitive behavioral therapy and acceptance and commitment therapy for anxiety disorders. Behaviour Research and Therapy. 2012; 50(7-8):469-78. [DOI:10.1016/j.brat.2012.04.007] [PMID]
Åkerblom S, Perrin S, Fischer MR, McCracken LM. The mediating role of acceptance in multidisciplinary cognitive-behavioral therapy for chronic pain. The Journal of Pain. 2015; 16(7):606-15. [DOI:10.1016/j.jpain.2015.03.007] [PMID]
Herbert MS, Afari N, Robinson JB, Listvinsky A, Bondi MW, Wetherell JL. Neuropsychological functioning and treatment outcomes in acceptance and commitment therapy for chronic pain. The Journal of Pain. 2018; 19(8):852-61. [DOI:10.1016/j.jpain.2018.02.008] [PMID]
Scott W, Hann KE, McCracken LM. A comprehensive examination of changes in psychological flexibility following acceptance and commitment therapy for chronic pain. Journal of Contemporary Psychotherapy. 2016; 46(3):139-48. [DOI:10.1007/s10879-016-9328-5] [PMID] [PMCID]
Martel ME, Dionne F, Scott W. The mediating role of pain acceptance in the relation between perceived injustice and chronic pain outcomes in a community sample. The Clinical Journal of Pain. 2017; 33(6):509-16. [DOI:10.1097/AJP.0000000000000427] [PMID]
Clementi MA, Kao GS, Monico E. Pain acceptance as a predictor of medical utilization and school absenteeism in adolescents with chronic pain. Journal of Pediatric Psychology. 2017; 43(3):294-302. [DOI:10.1093/jpepsy/jsx125] [PMID]
Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KM. Acceptance-and mindfulness-based interventions for the treatment of chronic pain: A meta-analytic review. Cognitive Behaviour Therapy. 2016; 45(1):5-31. [DOI:10.1080/16506073.2015.1098724] [PMID]
Turner J, Sherman K, Anderson M, Balderson B, Cook A, Cherkin D. Catastrophizing, pain self-efficacy, mindfulness, and acceptance: Relationships and changes among individuals receiving CBT, MBSR, or usual care for chronic back pain. The Journal of Pain. 2015; 16(4):96-107. [DOI:10.1016/j.jpain.2015.01.401]
Lillis J, Graham Thomas J, Seng EK, Lipton RB, Pavlovi JM, et al. Importance of pain acceptance in relation to headache disability and pain interference in women with migraine and overweight/obesity. Headache: The Journal of Head and Face Pain. 2017; 57(5):709-18. [DOI:10.1111/head.13058] [PMID] [PMCID]
Baranoff JA, Hanrahan SJ, Burke AL, Connor JP. Changes in acceptance in a low-intensity, group-based acceptance and commitment therapy (ACT) chronic pain intervention. International Journal of Behavioral Medicine. 2016; 23(1):30-8. [DOI:10.1007/s12529-015-9496-9] [PMID]
Goubert L, Crombez G, Van Damme S. The role of neuroticism, pain catastrophizing and pain-related fear in vigilance to pain: A structural equations approach. Pain. 2004; 107(3):234-41. [DOI:10.1016/j.pain.2003.11.005] [PMID]
Lin J, Paganini S, Sander L, Lüking M, Ebert DD, Buhrman M, et al. An internet-based intervention for chronic pain: A three-arm randomized controlled study of the effectiveness of guided and unguided acceptance and commitment therapy. Deutsches Ärzteblatt International. 2017; 114(41):681-97.
Simpson PA, Mars T, Esteves JE. A systematic review of randomised controlled trials using Acceptance and commitment therapy as an intervention in the management of non-malignant, chronic pain in adults. International Journal of Osteopathic Medicine. 2017; 24:18-31. [DOI:10.1016/j.ijosm.2017.03.001]
Article Type: Research Article |
Subject:
Special
Received: 2018/07/2 | Accepted: 2018/12/12 | Published: 2019/02/1
Received: 2018/07/2 | Accepted: 2018/12/12 | Published: 2019/02/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |