Volume 6, Issue 1 (Februrary 2019)
Avicenna J Neuro Psycho Physiology 2019, 6(1): 1-10 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shabani M, Ghari Saadati L. Comparison of the Effectiveness of Mindfulness-based Cognitive Therapy and Quality of Life Therapy on Perfectionism and Rumination in Patients with Migraine. Avicenna J Neuro Psycho Physiology 2019; 6 (1) :1-10
URL: http://ajnpp.umsha.ac.ir/article-1-131-en.html
URL: http://ajnpp.umsha.ac.ir/article-1-131-en.html
1- Department of Psychology, Faculty of Psychology and Education, Farhangian University, Torbat Heidarieh, Iran. , m.shabani52@yahoo.com
2- Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran.
2- Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran.
Full-Text [PDF 736 kb]
(1154 Downloads)
| Abstract (HTML) (1928 Views)
Full-Text: (1142 Views)
1. Introduction
Headache is the most prevalent neural symptom and one of the main medical complaints. Migraine headache is a specific invasive disorder with a one-side headache with or without visual or stomach-intestinal problems (eg nausea, vomiting, and photophobia). One probable cause of the headache is intracranial blood pressure [1]. Migraine is a sort of sensory processing disorder with wide branches within the central nervous system. Based on a general agreement, the nervous and vascular elements play a role in migraine. The nervous structures that affect migraines are the cerebral cortex and brainstem [2]. There are two general categories of migraine; migraine without aura and migraine with aura [3]. The latter, also known as classic migraine, is the less prevalent migraine and constitutes 15% to 20% of migraine cases. The difference between the classic migraine and migraine without aura is that in the former case, the patient experiences a series of neural disorders (e.g., the appearance of luminous spots and paresthesia) [4]. Migraine is also related to physical fatigue, emotional stresses, depression, and other psychological factors [5]. Migraine headaches may influence the patients’ work and social/private life with negative effects on their quality of life [6]. Recent studies have shown that migraine increases the risk of cardiac diseases, blockage, and hypertension. Authors have argued that the disease creates notable pressure and stress, affecting heartbeat and blood pressure [7]. In addition, psychological problems are common among patients with chronic headaches. A higher percentage of patients with migraine headaches also suffer from depression and anxiety disorders [8].
One of the prevalent patterns of migraine headaches is frequent intrusive thoughts that appear as rumination [9]. Abdolahi reported a relationship between rumination and migraine [10]. Rumination refers to the thoughts that tend to be repeatable and conscious and focused on a specific subject; they even appear in the absence of immediate and essential environmental stimuli [11]. Papajorjio and Wales showed that rumination is a long chain of repetitive, rotating, and self-centered thoughts and responses to primary negative thoughts [12]. Cognitive theory recommends that disastrous interpretation in the area of intrusive thoughts leads to the occurrence and persistence of such thoughts. The comprehensive analysis recommends that stimulus intrusive thoughts trigger specific automatic types of thoughts. According to this theory, an intrusive thought leads to mood disorder so that individual belief system finds the intrusive thoughts unacceptable and, consequently, triggers negative automatic thoughts [10]. Ruminative thoughts in response to painful experiences prolong and intensify depressed mood periods. In addition, rumination negatively tilts one’s thoughts so that an individual suffering from rumination tends to have lower problem-solving capability [12].
Several studies have focused on the biological and environmental effects and the psychological and social factors effective in the development of headaches. The results have supported the relationship between psychological and personality factors and headaches [13].
Abulghasemi showed a relationship between maladaptive perfectionism and the intensification of migraine headache [14]. Perfectionism is a set of high-performance standard featured with negative self-assessment, criticism, and self-blame. Ambition, discipline, excessive attention to details in daily activities, and excessive sensitivity to life affairs are psychological characteristics of perfectionists, which are also common in patients with migraine [15]. Shirzadi et al. showed a positive relationship between perfectionism and migraine headaches; the former would prepare the ground for psychosomatic disorders such as migraine headache [16]. Colotilo and Bromi reported that chronic pains and migraine experience explained 69% of the variance of disability in women with migraine [17]. Moreover, depression, migraine headaches, and chronic pain explained 8.64% of the variance of quality of life in individuals with migraine. Since the late 1970s, psychological treatments for headaches have drawn a great deal of attention. Research findings have also highlighted the effect of non-drug and cognitive and psychological methods for headache treatment [18-20]. In the same spirit, the present study surveys the effectiveness of quality of life-based treatment and mindfulness-based cognitive treatment.
Psychotherapy based on the improvement of the quality of life is a novel approach in positive psychology that includes continuous integration of cognitive therapy and positive psychology. It is consistent with Becks’ latest arrangement of cognitive therapy and cognitive theory of depression and psychopathology [21]. The treatment based on the quality of life is an approach to improve happiness. It is recommended for both clinical and non-clinical service takers [22]. It deals with and emphasizes different aspects of life, prevention, improvement of mental health, and marital satisfaction; it is one of the best approaches to improve the quality of life [23]. The quality of life therapy is based on a 5-way pattern of living conditions, attitudes, standards of fulfillment, importance, and overall satisfaction (CASIO) [24]. The objective of the treatment based on the quality of life is to improve professional self-care or inner enrichment and to prevent depression [22].
Another improvement was the introduction of a new approach by Tisdiel and Williams, which was based on a relationship between cognition, emotion, and mind. Their work led to a therapeutic cognitive approach based on mindfulness. The cognitive therapy based on mindfulness was a great advancement toward codifying the cognitive-behavioral therapeutic approach. Teaching mindfulness entails metacognition learning and new behavioral strategies to concentrate on the attention, to avoid rumination, and to tend to worrying responses, which leads to the expansion of new thoughts and attenuation of unwanted emotions. Mindfulness means paying attention in a specific and purposeful manner at the moment and without judgment [13]. Although, soothing is not the main objective of mindfulness, non-judgmental observation, internal negative events, and physiological arousal leads to it [25]. Mindfulness meditation activates an area of the brain that creates positive emotions and useful effects on the immunization function of the body [26]. Grisson, Brainard, and Roznzoik showed that mindfulness was effective in the attenuation of stress and treatment of physical and mental symptoms in individuals with chronic pains [27]. Regarding the paucity of studies in Iran and other countries on the effect of quality of life therapy and mindfulness-based cognitive therapy on the variables under study (migraine headache, perfectionism, and rumination), as well as comparing the two types of treatments, the present study tries to answer “If mindfulness-based cognitive therapy and the quality of life therapy are effective in perfectionism and rumination in patients with migraine?”.
2. Materials and Methods
Study Population, Sample Group, and Sampling Method
The present quasi-experimental study used a pretest-posttest design with 3 groups (2 experimental groups and 1 control group). Rumination was the dependent variable and it was measured for the two experimental groups and the control group before and after the implementation of the independent variables (mindfulness-based cognitive therapy and the quality of life therapy). The study population consisted of all patients with migraine headache referring to the hospitals and clinics of Torbat Heidarieh, Iran (June and July 2018). A sample group (N=45) was selected by the available sampling method and was randomly divided into 3 groups (n=15). The inclusion criteria included interest in participating in the study, education level ranged from high school diploma to bachelors’ degree, diagnosed by a specialist, at least 5 years history of the attack, migraine attack ranged from 4-72 hours, one-side headache attack, pulse headache, moderate to severe pain, the feeling of headache when climbing stairs or doing similar activities, nausea and vomiting, and photophobia and phonophobia. The exclusion criteria included diagnosis with psychological disorders, severe physical diseases, drug addiction or abuse, major medical disorders, neurological disorders, or chronic physical disease.
Research Tools
Multidimensional Perfectionism Scale
Frost’s Multidimensional Perfectionism Scale (FMPS) (1990) is based on a multi-aspect perfectionism model. This model was introduced with 6 elements of concerns about mistakes, doubts about actions, parental expectations, parental criticism, personal standards, and organization. The FMPS also contains 6 subscales, which are measured by 35 statements (Stober, 1998), including 2 positive and 4 negative aspects. The internal consistency of the Farsi version of the scale is 0.86 and 0.85, 0.72, 0.78, 0.47, 0.57, and 0.83 for the subscales of concerns about mistakes, doubts about actions, parental expectations, parental criticism, personal standards, and organization, respectively. Retest coefficients with the 1-week interval for the subscales of concerns about mistakes, doubts about actions, parental expectations, parental criticism, personal standards, and organization are 0.90, 0.084, 0.81, 0.79, 0.53, 0.85, and 0.83. Moreover, the correlative validity of FMPS based on its relevance to the positive and negative perfectionism scale is at an acceptable level [28].
Headache is the most prevalent neural symptom and one of the main medical complaints. Migraine headache is a specific invasive disorder with a one-side headache with or without visual or stomach-intestinal problems (eg nausea, vomiting, and photophobia). One probable cause of the headache is intracranial blood pressure [1]. Migraine is a sort of sensory processing disorder with wide branches within the central nervous system. Based on a general agreement, the nervous and vascular elements play a role in migraine. The nervous structures that affect migraines are the cerebral cortex and brainstem [2]. There are two general categories of migraine; migraine without aura and migraine with aura [3]. The latter, also known as classic migraine, is the less prevalent migraine and constitutes 15% to 20% of migraine cases. The difference between the classic migraine and migraine without aura is that in the former case, the patient experiences a series of neural disorders (e.g., the appearance of luminous spots and paresthesia) [4]. Migraine is also related to physical fatigue, emotional stresses, depression, and other psychological factors [5]. Migraine headaches may influence the patients’ work and social/private life with negative effects on their quality of life [6]. Recent studies have shown that migraine increases the risk of cardiac diseases, blockage, and hypertension. Authors have argued that the disease creates notable pressure and stress, affecting heartbeat and blood pressure [7]. In addition, psychological problems are common among patients with chronic headaches. A higher percentage of patients with migraine headaches also suffer from depression and anxiety disorders [8].
One of the prevalent patterns of migraine headaches is frequent intrusive thoughts that appear as rumination [9]. Abdolahi reported a relationship between rumination and migraine [10]. Rumination refers to the thoughts that tend to be repeatable and conscious and focused on a specific subject; they even appear in the absence of immediate and essential environmental stimuli [11]. Papajorjio and Wales showed that rumination is a long chain of repetitive, rotating, and self-centered thoughts and responses to primary negative thoughts [12]. Cognitive theory recommends that disastrous interpretation in the area of intrusive thoughts leads to the occurrence and persistence of such thoughts. The comprehensive analysis recommends that stimulus intrusive thoughts trigger specific automatic types of thoughts. According to this theory, an intrusive thought leads to mood disorder so that individual belief system finds the intrusive thoughts unacceptable and, consequently, triggers negative automatic thoughts [10]. Ruminative thoughts in response to painful experiences prolong and intensify depressed mood periods. In addition, rumination negatively tilts one’s thoughts so that an individual suffering from rumination tends to have lower problem-solving capability [12].
Several studies have focused on the biological and environmental effects and the psychological and social factors effective in the development of headaches. The results have supported the relationship between psychological and personality factors and headaches [13].
Abulghasemi showed a relationship between maladaptive perfectionism and the intensification of migraine headache [14]. Perfectionism is a set of high-performance standard featured with negative self-assessment, criticism, and self-blame. Ambition, discipline, excessive attention to details in daily activities, and excessive sensitivity to life affairs are psychological characteristics of perfectionists, which are also common in patients with migraine [15]. Shirzadi et al. showed a positive relationship between perfectionism and migraine headaches; the former would prepare the ground for psychosomatic disorders such as migraine headache [16]. Colotilo and Bromi reported that chronic pains and migraine experience explained 69% of the variance of disability in women with migraine [17]. Moreover, depression, migraine headaches, and chronic pain explained 8.64% of the variance of quality of life in individuals with migraine. Since the late 1970s, psychological treatments for headaches have drawn a great deal of attention. Research findings have also highlighted the effect of non-drug and cognitive and psychological methods for headache treatment [18-20]. In the same spirit, the present study surveys the effectiveness of quality of life-based treatment and mindfulness-based cognitive treatment.
Psychotherapy based on the improvement of the quality of life is a novel approach in positive psychology that includes continuous integration of cognitive therapy and positive psychology. It is consistent with Becks’ latest arrangement of cognitive therapy and cognitive theory of depression and psychopathology [21]. The treatment based on the quality of life is an approach to improve happiness. It is recommended for both clinical and non-clinical service takers [22]. It deals with and emphasizes different aspects of life, prevention, improvement of mental health, and marital satisfaction; it is one of the best approaches to improve the quality of life [23]. The quality of life therapy is based on a 5-way pattern of living conditions, attitudes, standards of fulfillment, importance, and overall satisfaction (CASIO) [24]. The objective of the treatment based on the quality of life is to improve professional self-care or inner enrichment and to prevent depression [22].
Another improvement was the introduction of a new approach by Tisdiel and Williams, which was based on a relationship between cognition, emotion, and mind. Their work led to a therapeutic cognitive approach based on mindfulness. The cognitive therapy based on mindfulness was a great advancement toward codifying the cognitive-behavioral therapeutic approach. Teaching mindfulness entails metacognition learning and new behavioral strategies to concentrate on the attention, to avoid rumination, and to tend to worrying responses, which leads to the expansion of new thoughts and attenuation of unwanted emotions. Mindfulness means paying attention in a specific and purposeful manner at the moment and without judgment [13]. Although, soothing is not the main objective of mindfulness, non-judgmental observation, internal negative events, and physiological arousal leads to it [25]. Mindfulness meditation activates an area of the brain that creates positive emotions and useful effects on the immunization function of the body [26]. Grisson, Brainard, and Roznzoik showed that mindfulness was effective in the attenuation of stress and treatment of physical and mental symptoms in individuals with chronic pains [27]. Regarding the paucity of studies in Iran and other countries on the effect of quality of life therapy and mindfulness-based cognitive therapy on the variables under study (migraine headache, perfectionism, and rumination), as well as comparing the two types of treatments, the present study tries to answer “If mindfulness-based cognitive therapy and the quality of life therapy are effective in perfectionism and rumination in patients with migraine?”.
2. Materials and Methods
Study Population, Sample Group, and Sampling Method
The present quasi-experimental study used a pretest-posttest design with 3 groups (2 experimental groups and 1 control group). Rumination was the dependent variable and it was measured for the two experimental groups and the control group before and after the implementation of the independent variables (mindfulness-based cognitive therapy and the quality of life therapy). The study population consisted of all patients with migraine headache referring to the hospitals and clinics of Torbat Heidarieh, Iran (June and July 2018). A sample group (N=45) was selected by the available sampling method and was randomly divided into 3 groups (n=15). The inclusion criteria included interest in participating in the study, education level ranged from high school diploma to bachelors’ degree, diagnosed by a specialist, at least 5 years history of the attack, migraine attack ranged from 4-72 hours, one-side headache attack, pulse headache, moderate to severe pain, the feeling of headache when climbing stairs or doing similar activities, nausea and vomiting, and photophobia and phonophobia. The exclusion criteria included diagnosis with psychological disorders, severe physical diseases, drug addiction or abuse, major medical disorders, neurological disorders, or chronic physical disease.
Research Tools
Multidimensional Perfectionism Scale
Frost’s Multidimensional Perfectionism Scale (FMPS) (1990) is based on a multi-aspect perfectionism model. This model was introduced with 6 elements of concerns about mistakes, doubts about actions, parental expectations, parental criticism, personal standards, and organization. The FMPS also contains 6 subscales, which are measured by 35 statements (Stober, 1998), including 2 positive and 4 negative aspects. The internal consistency of the Farsi version of the scale is 0.86 and 0.85, 0.72, 0.78, 0.47, 0.57, and 0.83 for the subscales of concerns about mistakes, doubts about actions, parental expectations, parental criticism, personal standards, and organization, respectively. Retest coefficients with the 1-week interval for the subscales of concerns about mistakes, doubts about actions, parental expectations, parental criticism, personal standards, and organization are 0.90, 0.084, 0.81, 0.79, 0.53, 0.85, and 0.83. Moreover, the correlative validity of FMPS based on its relevance to the positive and negative perfectionism scale is at an acceptable level [28].
Ahvaz Migraine Questionnaire
The questionnaire was designed and normalized by Najarian [29]. It includes 25 statements and is developed with the participation of 382 students at Shahid Chamran University and the Islamic Azad University of Ahvaz. The statements are designed based on 4-point Likert scale (never=1, rarely=2, sometimes=3, and most of the time=4). The questionnaire was used to determine prevalence and screen and select the sample group. Najarian measured the reliability of the tool through retest and internal consistency and obtained 0.8 and 0.91, respectively. Shirzadi Bistoni [16] measured the validity of the questionnaire, using the hospital anxiety and depression scale, hysteria, hypochondria, anxiety subscale, short-form of Minnesota multiphasic personality inventory, and Ahvaz aggression scale. The correlation coefficients were 0.49, 0.34, 0.36, 0.49, and 0.46, respectively, and all of them were significant (P=0.05). He also calculated the correlation coefficient of the Ahvaz migraine questionnaire, using the Ahvaz perfectionism scale and obtained r=0.50, which was significant (P<0.001).
Ruminative Response Scale
The scale was developed by Hoksma and Maro to measure negative mood reactions. The tool is comprised of two subscales of rumination responses and distraction responses, each of which is covered with 11 statements. The 22 statements of the scale are scored based on 4-point Likert scale (never=1, rarely=2, sometimes=3, and most of the time=4). Bagherinejad, Salehi, and Tabatabaie reported the reliability of 0.90 for the tool and 0.92 and 0.89 for the subscales, using Cronbach’s alpha [30]. The validity of the questionnaire was examined by finding a correlation of 0.65 at 0.001 level with the metacognitive belief questionnaire. The validity was confirmed. Tabibzadeh and Sepehrian Azar obtained the reliability of the tool, using Cronbach’s alpha of 0.80 [31].
Procedure
After securing the required permission from the research department and making an arrangement with the officials of hospitals and clinics located in Torbat Heidarieh, 45 participants were randomly selected from the patients with migraine referring to the health services facilities. Afterward, they were randomly divided into 3 groups each with 15 members (2 experimental groups and 1 control group). The first experimental group received quality of life therapy and the second one received mindfulness-based cognitive therapy. The control group received no intervention. Before and after the intervention, the participants filled out the research tools.
Data Analysis
The collected data were analyzed by SPSS v. 22, using descriptive statistics (Mid and Mean±SD) and inferential statistics (Analysis of covariance [ANCOVA] and independent t-test).
3. Results
Totally, 16 (35.6%) participants were men and 29 (64.4%) were women. In addition, 20 (44.4%) participants aged 22-29 years, 20 (44.44%) aged 30-39 years, and 5 (11.1%) aged 40-42 years. The age range of the participants was 22-42 years and the mean age was 32.22 years. Descriptive indices of perfectionism were measured in the control and experimental groups before and after the intervention. The mean score of perfectionism in the mindfulness group decreased by 5.67 after the intervention (91.4-85.7), the mean score of perfectionism in the quality of life group decreased by 2.67 (90.47-87.8), and the decrease in the control group was 1.34 (90.27-88.3). With regard to the element of perfectionism, there were differences between the pretest and posttest scores to some extent in all groups. Descriptive indices of rumination were measured at pretest and posttest stages for the control and experimental groups. Based on the indices, the mean score of rumination in the mindfulness treatment group decreased by 12 points (52.8-40.8) at the posttest stage and the mean score of rumination in quality of life group decreased by 9.26 points (54.33-45.07) at the posttest stage. The same figure increased by 4.33 points in the control group (53.07-57.4) at the posttest stage. In terms of the elements of rumination, the findings indicated differences among the mean scores at pretest and posttest stages in all groups.
The questionnaire was designed and normalized by Najarian [29]. It includes 25 statements and is developed with the participation of 382 students at Shahid Chamran University and the Islamic Azad University of Ahvaz. The statements are designed based on 4-point Likert scale (never=1, rarely=2, sometimes=3, and most of the time=4). The questionnaire was used to determine prevalence and screen and select the sample group. Najarian measured the reliability of the tool through retest and internal consistency and obtained 0.8 and 0.91, respectively. Shirzadi Bistoni [16] measured the validity of the questionnaire, using the hospital anxiety and depression scale, hysteria, hypochondria, anxiety subscale, short-form of Minnesota multiphasic personality inventory, and Ahvaz aggression scale. The correlation coefficients were 0.49, 0.34, 0.36, 0.49, and 0.46, respectively, and all of them were significant (P=0.05). He also calculated the correlation coefficient of the Ahvaz migraine questionnaire, using the Ahvaz perfectionism scale and obtained r=0.50, which was significant (P<0.001).
Ruminative Response Scale
The scale was developed by Hoksma and Maro to measure negative mood reactions. The tool is comprised of two subscales of rumination responses and distraction responses, each of which is covered with 11 statements. The 22 statements of the scale are scored based on 4-point Likert scale (never=1, rarely=2, sometimes=3, and most of the time=4). Bagherinejad, Salehi, and Tabatabaie reported the reliability of 0.90 for the tool and 0.92 and 0.89 for the subscales, using Cronbach’s alpha [30]. The validity of the questionnaire was examined by finding a correlation of 0.65 at 0.001 level with the metacognitive belief questionnaire. The validity was confirmed. Tabibzadeh and Sepehrian Azar obtained the reliability of the tool, using Cronbach’s alpha of 0.80 [31].
Procedure
After securing the required permission from the research department and making an arrangement with the officials of hospitals and clinics located in Torbat Heidarieh, 45 participants were randomly selected from the patients with migraine referring to the health services facilities. Afterward, they were randomly divided into 3 groups each with 15 members (2 experimental groups and 1 control group). The first experimental group received quality of life therapy and the second one received mindfulness-based cognitive therapy. The control group received no intervention. Before and after the intervention, the participants filled out the research tools.
Data Analysis
The collected data were analyzed by SPSS v. 22, using descriptive statistics (Mid and Mean±SD) and inferential statistics (Analysis of covariance [ANCOVA] and independent t-test).
3. Results
Totally, 16 (35.6%) participants were men and 29 (64.4%) were women. In addition, 20 (44.4%) participants aged 22-29 years, 20 (44.44%) aged 30-39 years, and 5 (11.1%) aged 40-42 years. The age range of the participants was 22-42 years and the mean age was 32.22 years. Descriptive indices of perfectionism were measured in the control and experimental groups before and after the intervention. The mean score of perfectionism in the mindfulness group decreased by 5.67 after the intervention (91.4-85.7), the mean score of perfectionism in the quality of life group decreased by 2.67 (90.47-87.8), and the decrease in the control group was 1.34 (90.27-88.3). With regard to the element of perfectionism, there were differences between the pretest and posttest scores to some extent in all groups. Descriptive indices of rumination were measured at pretest and posttest stages for the control and experimental groups. Based on the indices, the mean score of rumination in the mindfulness treatment group decreased by 12 points (52.8-40.8) at the posttest stage and the mean score of rumination in quality of life group decreased by 9.26 points (54.33-45.07) at the posttest stage. The same figure increased by 4.33 points in the control group (53.07-57.4) at the posttest stage. In terms of the elements of rumination, the findings indicated differences among the mean scores at pretest and posttest stages in all groups.
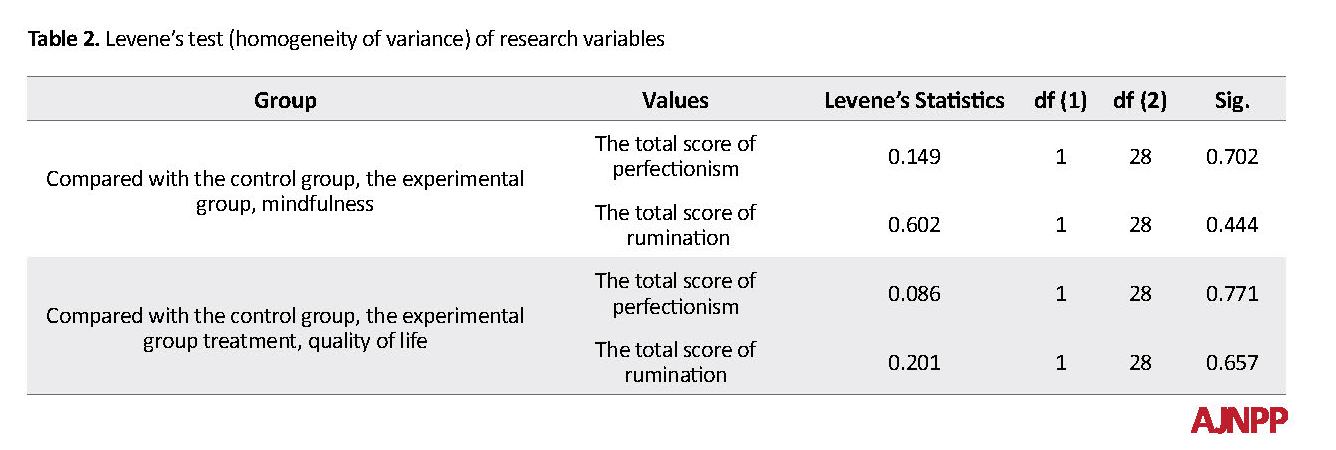
Data Analysis
The normal distribution of the data in the groups was ascertained, using the Shapiro Wilk test (P>0.01). The results of the Shapiro Wilk test show that the P-value of the two variables in the control and experimental groups is higher than 0.05 (P<0.05). In addition, skewness and kurtosis in all variables range from 2 and -2; i.e., normal distribution is supported. Therefore, non-parametric tests were used. In addition, equal variance condition was tested, using Levene’s test.
As presented in Table 2, the P-values of both variables are higher than 0.05. Therefore, the prerequisite of homogeneity of variances is met (P<0.05).
Hypothesis: There is a significant difference between the effectiveness of mindfulness-based cognitive therapy and quality of life therapy on perfectionism and rumination in patients with migraine.To test the hypothesis, the results of ANCOVA for the two experimental groups were compared.
The normal distribution of the data in the groups was ascertained, using the Shapiro Wilk test (P>0.01). The results of the Shapiro Wilk test show that the P-value of the two variables in the control and experimental groups is higher than 0.05 (P<0.05). In addition, skewness and kurtosis in all variables range from 2 and -2; i.e., normal distribution is supported. Therefore, non-parametric tests were used. In addition, equal variance condition was tested, using Levene’s test.
As presented in Table 2, the P-values of both variables are higher than 0.05. Therefore, the prerequisite of homogeneity of variances is met (P<0.05).
Hypothesis: There is a significant difference between the effectiveness of mindfulness-based cognitive therapy and quality of life therapy on perfectionism and rumination in patients with migraine.To test the hypothesis, the results of ANCOVA for the two experimental groups were compared.
As presented in Table 3, there was a significant difference between the effect size (η2) of the mindfulness-based cognitive therapy and quality of life therapy on perfectionism and rumination; that is, in the case of perfectionism, the former treatment is more effective (0.053 vs. 0.005) and in terms of rumination, the former treatment is more effective (0.312 vs. 0.266).
As presented in Table 4, the difference between the two treatment methods in terms of effectiveness in perfectionism and rumination was not significant (P>0.05).
4. Discussion
The effectiveness of mindfulness-based cognitive therapy and quality of life therapy on perfectionism and rumination in patients with migraine was examined. The results of ANCOVA supported the effect of both treatments on perfectionism and rumination. The two methods were significantly different in terms of effectiveness in perfectionism and rumination. The size effect of mindfulness-based cognitive therapy on perfectionism was higher than that of the quality of life therapy. These findings are consistent with Abdollahi et al., Azargon et al., Mansouri Shahd et al., and Melisa Biveli [9, 13, 31, 32]. Yusefi et al. showed that cognitive intervention based on mindfulness-based cognitive therapy was effective in rumination [33]. Abbas Abadi argued that cognitive intervention based on mindfulness was effective in rumination [34]. Moreover, Shahidi maintained that treatment based on mindfulness was effective in perfectionism [35].
Abdollahi et al. [10] showed that behavioral cognitive treatment was effective in attenuating rumination in patients with migraine, who suffered from the compulsory obsessive disorder. Mansourishad et al. demonstrated that behavioral mindfulness-based cognitive therapy was effective in the attenuation of migraine headache [32]. Yusefi et al. showed that mindfulness-based cognitive therapy was effective in rumination, metacognitive beliefs, and perfectionism in patients with obsessive through disorder. These studies have reported consistent results with the present research [24].
Mindfulness-based cognitive therapy helps the individual to concentrate on the moment rather than the future so that it increases awareness about one’s body by improving self-supervision. Such intervention leads to a notable decrease in psychological symptoms and higher self-care. On the other hand, people feel less motivated to control their environment, following the unexpected diagnosis of migraine [36]. Mindfulness practices create psychological functions and considerable changes in patients’ lives. By developing strategies to adapt to their situations and better defensive structures, individuals achieve higher mental welfare. Individuals also learn to positively reevaluate unwanted events such as a migraine.
Through learning coping skills in the face of stressful events, people learn to deal with such situations with self-confidence and optimistically. They tend to see things under control and, in general, use their information processing system in a more efficient way. Patients tend to blame themselves and lose their coping power when a part of their thoughts is focused on the idea that their lifestyle had led to the disease they suffer. Mindfulness-based cognitive therapy helps these individuals to experience emotions neither as positive nor negative [37]. In this way, the individual lets in and out the thoughts and emotions without struggling with them [38].
The first step in mindfulness treatment is the improvement of metacognitive awareness; ie reevaluating one’s thoughts and emotions and perceiving them as temporary events rather than reality. It is assumed that this metacognitive awareness leads to less rumination- repetition of negative thoughts- and in turn less catastrophic thinking, rumination, and other symptoms such as stress and ineffective/passive coping skills. These lead to an attenuation of migraine symptoms and a higher quality of life for the patients [39].
To elaborate on the difference between the mindfulness-based cognitive therapy and the quality of life therapy, the former significantly alleviates rumination and perfectionism as it is based on Beck’s pathological model and tries to evaluate the fundamental beliefs and assumptions that determine cognitive content in Beck’s theory. Therefore, an improvement in efficient attitudes following the treatment is quite expectable. Moreover, throughout mindfulness-based cognitive therapy, more cognitive changes happen in rumination and ineffective attitudes. These therapeutic changes mediate the symptoms of perfectionism. Mindfulness training, through thinking practices, enables the patients to see the negative ruminative responses in their brain more clearly and break the thought patterns. The quality of life therapy is based on the 5-path pattern CASIO [40] that supports the approach of satisfaction with life. However, the objective of mindfulness treatment is to improve professional self-care or inner richness and avoiding depression [22].
The main area of focus under the mindfulness approach is on improving metacognitive awareness and self-knowledge processes that support non-useful reactive and ruminative modes. Here, the effectiveness of mindfulness-based cognitive therapy on rumination and perfectionism was supported. Based on the results of this study, it is suggested that researchers evaluate the effect of mindfulness-based cognitive therapy on gender-specific migraine sufferers, as well as on other types of migraine. It is also suggested that health psychologists use mindfulness-based cognitive therapy to solve problems related to rumination and other mood disorders in migraine headaches. The limitations of this study include the small size that can challenge the validity of the findings and the use of self-report instruments.
5. Conclusion
The education based on reforming-based cognitions, replacing negative and intrusive thoughts with positive thoughts, and solving intrusive thoughts through neutralization, using mindfulness-based cognitive therapy and quality of life therapy led to a notable improvement in rumination, frequent intrusive thoughts, and perfectionism. In fact, changes in cognitive responses to pain, beliefs, and expectations are the main mechanisms of attenuation of headaches. Cognitions are related to emotional, physiological, and behavioral responses. Therefore, one’s thoughts affect the behavior by affecting physiological and emotional responses.
Ethical Considerations
Compliance with ethical guidelines
In this study, all relevant ethical principles, including the confidentiality of the questionnaires, the informed consent of the participants in the research, and the freedom to leave the research were observed. The study was approved by the Ethics Committee of the Islamic Azad University of Mashhad (Code: IR.IAU.MSHD.REC.1397.029).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
???
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
This article is based on the PhD dissertation of the Islamic Azad University of Mashhad. The authors of the article would like to thank the cooperation and assistance of all those, who helped us in this research.
References
Sadock B, Sadock V. Kaplan and Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 10th edition. Philadelphia: Lippincott Williams and Wilkins and Wolter Kluwer Health; 2009.
Coppola G, Pierelli F, Schoenenn J. Habituation and migraine. Neurobiology of Learning and Memory. 2008; 92:249-59. [DOI:10.1016/j.nlm.2008.07.006] [PMID]
Rocket T, Fernanda C, Oliveira E, Vanessa R, Merical L. Castro Nutrition. Reviews. 2012; 70:337-56. [DOI:10.1111/j.1753-4887.2012.00468.x] [PMID]
Fallahzadeh H, Heidari A, Hosseini H. The prevalence of migraine headache and tension in students in the middle school of Yazd. Journal of Iranian University of Medical Sciences. 2010; 17:61-52.
Ebrahimi F, Najmi Varzaneh F, Mohammadi Y, Razaghi Jahromi S, Tagh M. Types of tension and migraine headaches among medical staff in Sina Hospital, Tehran. Healing Khatam. 2018; 6(2):26-30. [DOI:10.29252/shefa.6.2.25]
Lipton RB, Stewart WF, Von Korff M. The burden of migraine. A review of cost to society. Pharmacoeconomics. 1994; 6(3):215-21. [DOI:10.2165/00019053-199406030-00005] [PMID]
Schwaiger J, Kiechl S, Stockner H, Knoflach M, Werner P, Rungger G, et al. Burden of atherosclerosis and risk of venous thromboembolism in patients with migraine. Neurology. 2008; 71(12):937-43. [DOI:10.1212/01.wnl.0000325918.48056.75] [PMID]
Amico D, Libro G, Prudenzano MP. Stress and chronic headache. The journal of Headache and Pain. 2000; 1(1):49-52. [DOI:10.1007/s101940070026] [PMCID]
Abdollahi M, Arab Nejad M, Farzaneh S, editors. The Effectiveness of Cognitive-Behavioral Therapy on Reducing Stomach Congestion in Migraine Patients with Obsessive Compulsive Disorder. 9th International Congress on Psychotherapy (Asian Summit on Cultural Values); 2015. 2015; iran.
Abdullahi M. The effectiveness of cognitive-behavioral education on reducing rhombeism in patients with migraine with obsessive compulsive disorder. iran2011.
Martin L, Tesser A, In JS. Toward a motivational and structural theory of ruminative thought. New York: Guilford Press; 1989.
Papageorgiou CC, Alevizos B, Ventouras E, Kontopantelis E, Uzunoglu N, Christodoulou G. Depressive Rumination: Nature, Theory, and Treatment. New York: Wiley; 2004.
Azargoon H, Kajbaf M, Molavi H, Abedi M. The effectiveness of mindfulness training on rhysis and depression in Isfahan University students. Daneshvar Behavior. 2009; 16(34):13-5.
Abolghasemi A, Jafari I, Ahmadi Taher Soltani M. Comparison of perfectionism, aggression and coping styles of patients with migraine headaches and tension with normal people. Journal of Kerman University of Medical Sciences. 2014; 21(2):162-73.
Waldie KE, Poulton R. Physical and psychological correlates of primary headache in young adulthood: A 26 year longitudinal study. J Neurol Neurosurg Psychiatry. 2002; 72(1):86-92. [DOI:10.1136/jnnp.72.1.86] [PMID] [PMCID]
Sherzadi M, Mehrabizadeh Arminand M, Haghighi J. Investigation of simple and multiple relationship between perfectionism, trait-state anxiety and depression with migraine headache in students. Journal of Educational Sciences and Psychology University of Shahid Chamran Ahwaz. 2003; 9(3,4):109-26.
Kolotylo CJ, Broome ME. Predicting disability and quality of life in a community-based sample of women with migraine headache. Pain management nursing: 0fficial journal of the American Society of Pain Management Nurses. 2000; 1(4):139-51. [DOI:10.1053/jpmn.2000.19344] [PMID]
Brown H, Newman C, Noad R, Weatherby S. Behavioural management of migraine. Ann Indian Acad Neurol. 2012; 15(Suppl 1):S78-82. [DOI:10.4103/0972-2327.100018] [PMID] [PMCID]
Nicholson RA, Buse DC, Andrasik F, Lipton RB. Nonpharmacologic treatments for migraine and tension-type headache: How to choose and when to use. Current Treatment Options in Neurology. 2011; 13(1):28-40. [DOI:10.1007/s11940-010-0102-9] [PMID]
Rahimian B, Besharat M. The effect of the program on the reduction of stress-relief on the severity of fibromyalgia. Contemporary Psychology. 2012; 14:28-15.
Padash Z, Fatehizadeh M, Abedi M, Izidikhah Z. Effectiveness of treatment based on improving the quality of life on marital satisfaction. Journal of Research in Behavioral Sciences. 2012; 10(5):363-72.
Frisch M. Psychotherapy based on improving quality of life. Tehran: Arjmand Publishing; 2012.
Rostami M, Abolqasemi A, Narimani M. The effectiveness of treatment based on improving the quality of life in the quality of life of couples incompatible. Journal of Science and Technology. 2016;15(1):26-35. [DOI:10.11594/jtls.06.01.07]
Yousefi E, Azadeh M, Majlesi Z, Salehi A. The effectiveness of Mindfulness-Based Cognitive Therapy (MBCT) intervention on mental and perfectionism in patients with obsessive-compulsive disorder in Isfahan Province. International Journal of Humanities and Cultural Studies. 2016; Special Issue: 1943-51.
Borkovec TD. Life in the future versus life in the present. Clinical Psychology: Science and Practice. 2002; 9(1):76-80. [DOI:10.1093/clipsy.9.1.76]
Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003; 65(4):564-70. [DOI:10.1097/01.PSY.0000077505.67574.E3] [PMID]
Greeson J, Brainard G, Rosenzweig S. Mindfulness based stress reduction quality of life in a heterogeneous patient population. General Hospital Psychiatry. 2003; 23:183-92. [DOI:10.1016/S0163-8343(01)00149-9]
Bitaraf S, Shoori MR, Hakim Javadi M. Social phobia, parenting styles and perfectionism, evolutionary psychology. Iranian Psychologists. 2010; 7(25):75-82.
Najjarian B, Attari Y, Zargar Y. Compilation and scale validation for perfectionism. Journal of Faculty of Education and Psychology University of Shahid Chamran Ahvaz. 1999; 3(5):43-58.
Bagherinejad M, Salehi Fadardi J, Tabatabaei M. Relationship between rumination and depression in a sample of Iranian students. Studies In Education & Psychology. 2010; 11(1):21-38.
Day AM, Thorn BE. Mindfulness-based cognitive therapy for headache pain: An evaluation of the long-term maintenance of effects. Complementary Therapies in Medicine. 2017; 33:94-8. [DOI:10.1016/j.ctim.2017.06.009] [PMID]
Mansourishad H, Togha M, Borjali A, Karimi R. Effectiveness of mindfulness-based cognitive-behavioral therapy on relieving migraine headaches. Archives of Neuroscience. 2017; 4(4):e58028. [DOI:10.5812/archneurosci.58028]
Yusufpour N, Ahi Q, Nasri M. Psychotherapy based on improving quality of life on anxiety in patients with complicated mourning. Journal of Birjand University of Medical Sciences. 2015; 22(2 ):153-45.
Abbas Abadi S. Effectiveness of cognitive-based cognitive therapy on perfectionism. iran2014.
Afshari A, Ghaffari M. Relationship between metacognition and perfectionism with duration of methadone maintenance treatment in addicts referred to addiction treatment centers. Feyz. 2019; 23(2):177-84.
Narimani T, Douraghi M, Owlia P, Rastegar A, Esghaei M, Nasr B, et al. Comparison of perfectionism and rumination among people with migraines. 4th national conference on sustainable development in psychology and social studies, and social studies; 2016. iran.
Emanuel SA, Updegraff JA, Kalmbach DA, Ciesla JA . The role of mindfulness in affective forecasting. Personality and Individual Differences. 2010; In Press:1-4. [DOI:10.1016/j.paid.2010.06.012]
Babapour J. The relationship of metacognition components and mindfulness to obsessive beliefs among students. JOURNAL OF SCHOOL PSYCHOLOGY. 2014;1(4):23-38.
Zomordi S, Rasoulzadeh Tabatabaei SK. Comparison of the Effectiveness of Cognitive Behavioral Therapy and Mindfulness-Based Therapy on Improving Quality of Life in Patients with Irritable Bowel Syndrome. Quarterly Journal of Clinical Psychology. 2013;13(4):64-87.
Kabat-Zinn J. Coming to our senses: Healing ourselves and the world through mindfulness. New York: Hachette Books; 2006.
As presented in Table 4, the difference between the two treatment methods in terms of effectiveness in perfectionism and rumination was not significant (P>0.05).
4. Discussion
The effectiveness of mindfulness-based cognitive therapy and quality of life therapy on perfectionism and rumination in patients with migraine was examined. The results of ANCOVA supported the effect of both treatments on perfectionism and rumination. The two methods were significantly different in terms of effectiveness in perfectionism and rumination. The size effect of mindfulness-based cognitive therapy on perfectionism was higher than that of the quality of life therapy. These findings are consistent with Abdollahi et al., Azargon et al., Mansouri Shahd et al., and Melisa Biveli [9, 13, 31, 32]. Yusefi et al. showed that cognitive intervention based on mindfulness-based cognitive therapy was effective in rumination [33]. Abbas Abadi argued that cognitive intervention based on mindfulness was effective in rumination [34]. Moreover, Shahidi maintained that treatment based on mindfulness was effective in perfectionism [35].
Abdollahi et al. [10] showed that behavioral cognitive treatment was effective in attenuating rumination in patients with migraine, who suffered from the compulsory obsessive disorder. Mansourishad et al. demonstrated that behavioral mindfulness-based cognitive therapy was effective in the attenuation of migraine headache [32]. Yusefi et al. showed that mindfulness-based cognitive therapy was effective in rumination, metacognitive beliefs, and perfectionism in patients with obsessive through disorder. These studies have reported consistent results with the present research [24].
Mindfulness-based cognitive therapy helps the individual to concentrate on the moment rather than the future so that it increases awareness about one’s body by improving self-supervision. Such intervention leads to a notable decrease in psychological symptoms and higher self-care. On the other hand, people feel less motivated to control their environment, following the unexpected diagnosis of migraine [36]. Mindfulness practices create psychological functions and considerable changes in patients’ lives. By developing strategies to adapt to their situations and better defensive structures, individuals achieve higher mental welfare. Individuals also learn to positively reevaluate unwanted events such as a migraine.
Through learning coping skills in the face of stressful events, people learn to deal with such situations with self-confidence and optimistically. They tend to see things under control and, in general, use their information processing system in a more efficient way. Patients tend to blame themselves and lose their coping power when a part of their thoughts is focused on the idea that their lifestyle had led to the disease they suffer. Mindfulness-based cognitive therapy helps these individuals to experience emotions neither as positive nor negative [37]. In this way, the individual lets in and out the thoughts and emotions without struggling with them [38].
The first step in mindfulness treatment is the improvement of metacognitive awareness; ie reevaluating one’s thoughts and emotions and perceiving them as temporary events rather than reality. It is assumed that this metacognitive awareness leads to less rumination- repetition of negative thoughts- and in turn less catastrophic thinking, rumination, and other symptoms such as stress and ineffective/passive coping skills. These lead to an attenuation of migraine symptoms and a higher quality of life for the patients [39].
To elaborate on the difference between the mindfulness-based cognitive therapy and the quality of life therapy, the former significantly alleviates rumination and perfectionism as it is based on Beck’s pathological model and tries to evaluate the fundamental beliefs and assumptions that determine cognitive content in Beck’s theory. Therefore, an improvement in efficient attitudes following the treatment is quite expectable. Moreover, throughout mindfulness-based cognitive therapy, more cognitive changes happen in rumination and ineffective attitudes. These therapeutic changes mediate the symptoms of perfectionism. Mindfulness training, through thinking practices, enables the patients to see the negative ruminative responses in their brain more clearly and break the thought patterns. The quality of life therapy is based on the 5-path pattern CASIO [40] that supports the approach of satisfaction with life. However, the objective of mindfulness treatment is to improve professional self-care or inner richness and avoiding depression [22].
The main area of focus under the mindfulness approach is on improving metacognitive awareness and self-knowledge processes that support non-useful reactive and ruminative modes. Here, the effectiveness of mindfulness-based cognitive therapy on rumination and perfectionism was supported. Based on the results of this study, it is suggested that researchers evaluate the effect of mindfulness-based cognitive therapy on gender-specific migraine sufferers, as well as on other types of migraine. It is also suggested that health psychologists use mindfulness-based cognitive therapy to solve problems related to rumination and other mood disorders in migraine headaches. The limitations of this study include the small size that can challenge the validity of the findings and the use of self-report instruments.
5. Conclusion
The education based on reforming-based cognitions, replacing negative and intrusive thoughts with positive thoughts, and solving intrusive thoughts through neutralization, using mindfulness-based cognitive therapy and quality of life therapy led to a notable improvement in rumination, frequent intrusive thoughts, and perfectionism. In fact, changes in cognitive responses to pain, beliefs, and expectations are the main mechanisms of attenuation of headaches. Cognitions are related to emotional, physiological, and behavioral responses. Therefore, one’s thoughts affect the behavior by affecting physiological and emotional responses.
Ethical Considerations
Compliance with ethical guidelines
In this study, all relevant ethical principles, including the confidentiality of the questionnaires, the informed consent of the participants in the research, and the freedom to leave the research were observed. The study was approved by the Ethics Committee of the Islamic Azad University of Mashhad (Code: IR.IAU.MSHD.REC.1397.029).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
???
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
This article is based on the PhD dissertation of the Islamic Azad University of Mashhad. The authors of the article would like to thank the cooperation and assistance of all those, who helped us in this research.
References
Sadock B, Sadock V. Kaplan and Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 10th edition. Philadelphia: Lippincott Williams and Wilkins and Wolter Kluwer Health; 2009.
Coppola G, Pierelli F, Schoenenn J. Habituation and migraine. Neurobiology of Learning and Memory. 2008; 92:249-59. [DOI:10.1016/j.nlm.2008.07.006] [PMID]
Rocket T, Fernanda C, Oliveira E, Vanessa R, Merical L. Castro Nutrition. Reviews. 2012; 70:337-56. [DOI:10.1111/j.1753-4887.2012.00468.x] [PMID]
Fallahzadeh H, Heidari A, Hosseini H. The prevalence of migraine headache and tension in students in the middle school of Yazd. Journal of Iranian University of Medical Sciences. 2010; 17:61-52.
Ebrahimi F, Najmi Varzaneh F, Mohammadi Y, Razaghi Jahromi S, Tagh M. Types of tension and migraine headaches among medical staff in Sina Hospital, Tehran. Healing Khatam. 2018; 6(2):26-30. [DOI:10.29252/shefa.6.2.25]
Lipton RB, Stewart WF, Von Korff M. The burden of migraine. A review of cost to society. Pharmacoeconomics. 1994; 6(3):215-21. [DOI:10.2165/00019053-199406030-00005] [PMID]
Schwaiger J, Kiechl S, Stockner H, Knoflach M, Werner P, Rungger G, et al. Burden of atherosclerosis and risk of venous thromboembolism in patients with migraine. Neurology. 2008; 71(12):937-43. [DOI:10.1212/01.wnl.0000325918.48056.75] [PMID]
Amico D, Libro G, Prudenzano MP. Stress and chronic headache. The journal of Headache and Pain. 2000; 1(1):49-52. [DOI:10.1007/s101940070026] [PMCID]
Abdollahi M, Arab Nejad M, Farzaneh S, editors. The Effectiveness of Cognitive-Behavioral Therapy on Reducing Stomach Congestion in Migraine Patients with Obsessive Compulsive Disorder. 9th International Congress on Psychotherapy (Asian Summit on Cultural Values); 2015. 2015; iran.
Abdullahi M. The effectiveness of cognitive-behavioral education on reducing rhombeism in patients with migraine with obsessive compulsive disorder. iran2011.
Martin L, Tesser A, In JS. Toward a motivational and structural theory of ruminative thought. New York: Guilford Press; 1989.
Papageorgiou CC, Alevizos B, Ventouras E, Kontopantelis E, Uzunoglu N, Christodoulou G. Depressive Rumination: Nature, Theory, and Treatment. New York: Wiley; 2004.
Azargoon H, Kajbaf M, Molavi H, Abedi M. The effectiveness of mindfulness training on rhysis and depression in Isfahan University students. Daneshvar Behavior. 2009; 16(34):13-5.
Abolghasemi A, Jafari I, Ahmadi Taher Soltani M. Comparison of perfectionism, aggression and coping styles of patients with migraine headaches and tension with normal people. Journal of Kerman University of Medical Sciences. 2014; 21(2):162-73.
Waldie KE, Poulton R. Physical and psychological correlates of primary headache in young adulthood: A 26 year longitudinal study. J Neurol Neurosurg Psychiatry. 2002; 72(1):86-92. [DOI:10.1136/jnnp.72.1.86] [PMID] [PMCID]
Sherzadi M, Mehrabizadeh Arminand M, Haghighi J. Investigation of simple and multiple relationship between perfectionism, trait-state anxiety and depression with migraine headache in students. Journal of Educational Sciences and Psychology University of Shahid Chamran Ahwaz. 2003; 9(3,4):109-26.
Kolotylo CJ, Broome ME. Predicting disability and quality of life in a community-based sample of women with migraine headache. Pain management nursing: 0fficial journal of the American Society of Pain Management Nurses. 2000; 1(4):139-51. [DOI:10.1053/jpmn.2000.19344] [PMID]
Brown H, Newman C, Noad R, Weatherby S. Behavioural management of migraine. Ann Indian Acad Neurol. 2012; 15(Suppl 1):S78-82. [DOI:10.4103/0972-2327.100018] [PMID] [PMCID]
Nicholson RA, Buse DC, Andrasik F, Lipton RB. Nonpharmacologic treatments for migraine and tension-type headache: How to choose and when to use. Current Treatment Options in Neurology. 2011; 13(1):28-40. [DOI:10.1007/s11940-010-0102-9] [PMID]
Rahimian B, Besharat M. The effect of the program on the reduction of stress-relief on the severity of fibromyalgia. Contemporary Psychology. 2012; 14:28-15.
Padash Z, Fatehizadeh M, Abedi M, Izidikhah Z. Effectiveness of treatment based on improving the quality of life on marital satisfaction. Journal of Research in Behavioral Sciences. 2012; 10(5):363-72.
Frisch M. Psychotherapy based on improving quality of life. Tehran: Arjmand Publishing; 2012.
Rostami M, Abolqasemi A, Narimani M. The effectiveness of treatment based on improving the quality of life in the quality of life of couples incompatible. Journal of Science and Technology. 2016;15(1):26-35. [DOI:10.11594/jtls.06.01.07]
Yousefi E, Azadeh M, Majlesi Z, Salehi A. The effectiveness of Mindfulness-Based Cognitive Therapy (MBCT) intervention on mental and perfectionism in patients with obsessive-compulsive disorder in Isfahan Province. International Journal of Humanities and Cultural Studies. 2016; Special Issue: 1943-51.
Borkovec TD. Life in the future versus life in the present. Clinical Psychology: Science and Practice. 2002; 9(1):76-80. [DOI:10.1093/clipsy.9.1.76]
Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003; 65(4):564-70. [DOI:10.1097/01.PSY.0000077505.67574.E3] [PMID]
Greeson J, Brainard G, Rosenzweig S. Mindfulness based stress reduction quality of life in a heterogeneous patient population. General Hospital Psychiatry. 2003; 23:183-92. [DOI:10.1016/S0163-8343(01)00149-9]
Bitaraf S, Shoori MR, Hakim Javadi M. Social phobia, parenting styles and perfectionism, evolutionary psychology. Iranian Psychologists. 2010; 7(25):75-82.
Najjarian B, Attari Y, Zargar Y. Compilation and scale validation for perfectionism. Journal of Faculty of Education and Psychology University of Shahid Chamran Ahvaz. 1999; 3(5):43-58.
Bagherinejad M, Salehi Fadardi J, Tabatabaei M. Relationship between rumination and depression in a sample of Iranian students. Studies In Education & Psychology. 2010; 11(1):21-38.
Day AM, Thorn BE. Mindfulness-based cognitive therapy for headache pain: An evaluation of the long-term maintenance of effects. Complementary Therapies in Medicine. 2017; 33:94-8. [DOI:10.1016/j.ctim.2017.06.009] [PMID]
Mansourishad H, Togha M, Borjali A, Karimi R. Effectiveness of mindfulness-based cognitive-behavioral therapy on relieving migraine headaches. Archives of Neuroscience. 2017; 4(4):e58028. [DOI:10.5812/archneurosci.58028]
Yusufpour N, Ahi Q, Nasri M. Psychotherapy based on improving quality of life on anxiety in patients with complicated mourning. Journal of Birjand University of Medical Sciences. 2015; 22(2 ):153-45.
Abbas Abadi S. Effectiveness of cognitive-based cognitive therapy on perfectionism. iran2014.
Afshari A, Ghaffari M. Relationship between metacognition and perfectionism with duration of methadone maintenance treatment in addicts referred to addiction treatment centers. Feyz. 2019; 23(2):177-84.
Narimani T, Douraghi M, Owlia P, Rastegar A, Esghaei M, Nasr B, et al. Comparison of perfectionism and rumination among people with migraines. 4th national conference on sustainable development in psychology and social studies, and social studies; 2016. iran.
Emanuel SA, Updegraff JA, Kalmbach DA, Ciesla JA . The role of mindfulness in affective forecasting. Personality and Individual Differences. 2010; In Press:1-4. [DOI:10.1016/j.paid.2010.06.012]
Babapour J. The relationship of metacognition components and mindfulness to obsessive beliefs among students. JOURNAL OF SCHOOL PSYCHOLOGY. 2014;1(4):23-38.
Zomordi S, Rasoulzadeh Tabatabaei SK. Comparison of the Effectiveness of Cognitive Behavioral Therapy and Mindfulness-Based Therapy on Improving Quality of Life in Patients with Irritable Bowel Syndrome. Quarterly Journal of Clinical Psychology. 2013;13(4):64-87.
Kabat-Zinn J. Coming to our senses: Healing ourselves and the world through mindfulness. New York: Hachette Books; 2006.
Article Type: Research Article |
Subject:
Clinical Psychology
Received: 2018/07/10 | Accepted: 2018/12/25 | Published: 2019/02/1
Received: 2018/07/10 | Accepted: 2018/12/25 | Published: 2019/02/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |