Volume 8, Issue 1 (February 2021)
Avicenna J Neuro Psycho Physiology 2021, 8(1): 39-44 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yazdani M, Khalatbari J, Ghorban Shiroudi S, Rahmani M A. Comparison of the Effectiveness of Compassion-Focused Therapy and Attachment-Based Compassion Therapy on Blood Glucose Level and Medication Adherence in Diabetics. Avicenna J Neuro Psycho Physiology 2021; 8 (1) :39-44
URL: http://ajnpp.umsha.ac.ir/article-1-274-en.html
URL: http://ajnpp.umsha.ac.ir/article-1-274-en.html
1- Ph.D. Candidate of Health Psychology, Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran
2- Associate Professor, Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran ,javadkhalatbaripsy2@gmail.com
3- Associate Professor, Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran
4- Assistant Professor, Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran
2- Associate Professor, Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran ,
3- Associate Professor, Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran
4- Assistant Professor, Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran
Full-Text [PDF 1623 kb]
(490 Downloads)
| Abstract (HTML) (1332 Views)
Table 1. Mean and standard deviation of research variables
Table 2. Results of mixed analysis of variance with intragroup and intergroup factors regarding the blood glucose level variable

Figure 1. Adjusted means of blood glucose level in both experimental and control groups during the studied phases
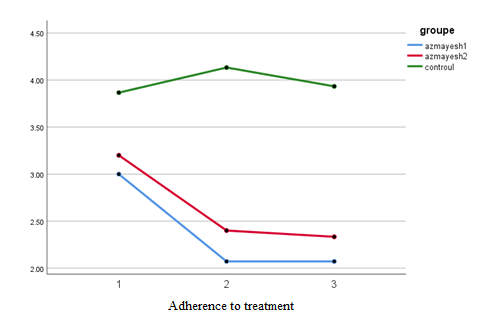
Figure 2. Adjusted means of medication adherence scores in both experimental and control groups during the studied phases
Full-Text: (714 Views)
Background
Diabetes is the most predominant metabolic disease that is characterized by high blood glucose, impaired carbohydrate, fat, and protein metabolism, and impairment in the secretion or function of insulin. The chronic nature of diabetes impacts the body, mind, and individual and social functions of patients [1]. Diabetes is a serious public health problem that reduces the quality of life of patients. It can lead to acute and chronic complications and is considered the main cause of debility and death in many countries. According to previous studies, diabetes has also a higher occurrence in Iran [2]. Diabetes mellitus is one of the prevalent chronic diseases that threaten the mental health of individuals [3].
The progressive increase of the incidence and prevalence of chronic diseases around the globe, higher rates of mortality, growing costs of taking care of these patients, and especially the vital role of psychological factors in the onset, persistence, and exacerbation of symptoms have led to a greater emphasis on psychological dimensions [4-6]. There are various types of psychological interventions that can significantly help to control blood glucose [7]. Various factors influence psychological problems, such as anxiety, depression, and low quality of life; one of these factors is the component of therapy adherence.
Therapy adherence is defined as the degree that one's behavior is in line with health or therapy directives [8]. In type 2 diabetes, more than 95% of the therapy process is accomplished by the patient, and the therapy group has little control over the patient in the intervals between visits [9]. It has been reported in the performed studies that 23-93% of diabetics do not follow therapy guidelines while following therapy is one of the essential factors in controlling the disease. Accordingly, there is a high positive correlation between the rate of therapy adherence and maintenance of optimal blood glucose metabolism [10].
Nowadays, it is a common belief that a biopsychosocial approach is required to treat and control this disease in a way that any change in the lifestyle and adherence to therapy directives can reduce diabetes incidence and help the patients control it by 85% [11]. Therefore, the term comprehensive care is employed in its therapy in order to attract the required attention to the fact that diabetes treatment is more than the control of blood glucose and must include the influential psychosocial personality factors as well [12]. The reason is that those with poor mental health do not have enough motivation and emotional strength to manage their diabetes [13].
Non-adherence to the medication regimen in diabetic patients is associated with frequent hospitalizations, lack of reception of therapy resources, high medical costs, and frequent doctor visits. Mortality rates in patients who do not adhere to their medication are twice as high as that of other patients [14-18].
Compassion therapy is one of the third-wave psychotherapies used along with mindfulness during recent years. According to attachment style, this model describes the concept of psychoanalysis based on which the relationships of children with their parents influence their intrapersonal relationships and self-image [19]. Attachment-based compassion therapy (ABCT) is a compassionate protocol that is used in both the general population as well as medical and psychiatric situations. It is based on basic psychological structures that explain interpersonal relationships [20].
This intervention includes a compassion training program that focuses on strengthening the ability of patients to be cautious and affectionate with themselves, their experiences, and the experiences of the suffering of others [21]. This therapy aims to assess the effectiveness of this improvement protocol and self-compassion and also determine what enhancements in self-compassion are mediators of change of attachment styles. Based on the results of a study performed by Mayte Navarro-Gil et al., ABCT was significantly effective in the improvement of self-compassion [22].
However, no study has been performed about the effect of CFT and ABCT on the psychological treatment of diabetics.
Objectives
This study aimed to compare the effectiveness of CFT and ABCT on the blood glucose level following therapy in patients with diabetes. The present study tried to find out whether compassion-focused therapy (CFT) and ABCT influence blood glucose level and medication adherence in diabetics or not.
Materials and Methods
This quasi-experimental study was conducted based on a pretest and posttest design with two experimental and one control groups. The statistical population of this research included a total number of 300 individuals with diabetes referred to
the Alborz Diabetes Association, Alborz, Iran. Regarding the sampling, at first, the researcher participated in the conferences of the Diabetes Association and delivered a speech about the goals and characteristics of the mentioned course and the inclusion criteria of this research project. Subsequently, the researcher collected the contact numbers of the volunteers.
Finally, 45 out of the 300 patients were invited to participate in the study through random assignment. The inclusion criteria in this study were 1) age range of 30-65 years, 2) minimum reading and writing ability, and 3) written confirmation of the disease by a qualified physician and based on the results of diagnostic tests. Moreover, the exclusion criteria were infliction with severe medical complications
of diabetes and consumption of psychotropic medication or medication abuse.
The first experimental group received 10 two-h sessions of CFT while the second group received eight two-and-half-h sessions of ABCT. It must be noted that the control group did not receive any intervention during this period. All participants were randomly assigned to three groups with equal numbers and written informed consent was obtained from the participants. In addition, pretest assessments were performed on all the participants.
Medication adherence scale (MAS)
Morisky's medication adherence questionnaire includes seven two-point options (Yes (0), No (1)) and one five-point option ranging from never (0) to always (4). A score of six or higher on this scale shows optimal medication adherence [20]. This questionnaire was translated into Persian for the first time by Bakaian [21] and its validity and reliability were confirmed. Reliability of this questionnaire was calculated at 0.89 by Cronbach's alpha coefficient.
Hemoglobin A1c Blood Test
The (Hemoglobin A1c) HbA1c is a protein that has been clinically recognized as the most important indicator of long-term blood control monitoring. This test measures the average blood glucose level for the preceding two to three months [22]. In fact, the effect of therapy and improvement in blood glucose control is manifested in HbA1c reduction [23]. This indicator is reported as a percentage and is interpretable based on the normal range which is specified by each laboratory.
First, a blood test was performed on the experimental groups; afterward, they were asked to complete a medication adherence questionnaire as well as a consent form for participation in this research. Subsequently, they underwent CFT and ABCT in group form during weekly sessions. The CFT included 10 sessions of self-compassion therapy based on the concepts of Gilbert (2010).
Attachment-based compassion therapy
This therapy includes eight two-and-half-hour sessions that include mindfulness and compassion training, such as receiving and offering love and compassion to friends, people who seem suspicious, strangers, and themselves. This program includes daily homework that lasts approximately 15-20 min. Moreover, it includes eight sessions as follows: 1) preparation of individuals for compassionate care with love, 2) discovery of the world of self-compassion, 3) development of a compassionate world, 4) comprehension of relationships with compassion, 5) development of one’s own self (the importance of love towards themselves and others), 6) advanced compassion 1 (forgiveness), 7) advanced compassion 2 (adaptation of the form of attachment and examination of different relationships), and 8) beyond compassion: sobriety and serenity.
At the end of the intervention program, the HbA1c levels of blood in all three groups were re-evaluated, and all individuals completed a post-test medication adherence questionnaire. Analysis of covariance was used to analyze the data and to determine the effectiveness of CFT training and ABCT on medication adherence and control of blood glucose in diabetic patients.
The collected data were analyzed in SPSS software (version 22) using descriptive statistical methods, such as mean, standard deviation, and analysis of Covariance. Moreover, Levene’s test was used to examine the assumption of variance equality of variables. In addition, the normality of distributing scores in the society was observed using the Skewness and Kurtosis tests.
Results
Based on the results, 10 (71%), 11 (73%), and 9 (60%) subjects in the first and second experimental, and control groups were female, respectively. It must be noted that each research group consisted of 15 participants. The mean, standard deviation, blood glucose levels, and medication adherence scores were calculated and the results are summarized in Table 1.
Based on Table 2, considering the intragroup factor, the calculated F value was significant for the effect of phases (i.e., pre-test, post-test, and follow-up) at a level smaller than 0.01 (Eta= 0.32, F=19.72, P<0.0001). As a result, there was a
The progressive increase of the incidence and prevalence of chronic diseases around the globe, higher rates of mortality, growing costs of taking care of these patients, and especially the vital role of psychological factors in the onset, persistence, and exacerbation of symptoms have led to a greater emphasis on psychological dimensions [4-6]. There are various types of psychological interventions that can significantly help to control blood glucose [7]. Various factors influence psychological problems, such as anxiety, depression, and low quality of life; one of these factors is the component of therapy adherence.
Therapy adherence is defined as the degree that one's behavior is in line with health or therapy directives [8]. In type 2 diabetes, more than 95% of the therapy process is accomplished by the patient, and the therapy group has little control over the patient in the intervals between visits [9]. It has been reported in the performed studies that 23-93% of diabetics do not follow therapy guidelines while following therapy is one of the essential factors in controlling the disease. Accordingly, there is a high positive correlation between the rate of therapy adherence and maintenance of optimal blood glucose metabolism [10].
Nowadays, it is a common belief that a biopsychosocial approach is required to treat and control this disease in a way that any change in the lifestyle and adherence to therapy directives can reduce diabetes incidence and help the patients control it by 85% [11]. Therefore, the term comprehensive care is employed in its therapy in order to attract the required attention to the fact that diabetes treatment is more than the control of blood glucose and must include the influential psychosocial personality factors as well [12]. The reason is that those with poor mental health do not have enough motivation and emotional strength to manage their diabetes [13].
Non-adherence to the medication regimen in diabetic patients is associated with frequent hospitalizations, lack of reception of therapy resources, high medical costs, and frequent doctor visits. Mortality rates in patients who do not adhere to their medication are twice as high as that of other patients [14-18].
Compassion therapy is one of the third-wave psychotherapies used along with mindfulness during recent years. According to attachment style, this model describes the concept of psychoanalysis based on which the relationships of children with their parents influence their intrapersonal relationships and self-image [19]. Attachment-based compassion therapy (ABCT) is a compassionate protocol that is used in both the general population as well as medical and psychiatric situations. It is based on basic psychological structures that explain interpersonal relationships [20].
This intervention includes a compassion training program that focuses on strengthening the ability of patients to be cautious and affectionate with themselves, their experiences, and the experiences of the suffering of others [21]. This therapy aims to assess the effectiveness of this improvement protocol and self-compassion and also determine what enhancements in self-compassion are mediators of change of attachment styles. Based on the results of a study performed by Mayte Navarro-Gil et al., ABCT was significantly effective in the improvement of self-compassion [22].
However, no study has been performed about the effect of CFT and ABCT on the psychological treatment of diabetics.
Objectives
This study aimed to compare the effectiveness of CFT and ABCT on the blood glucose level following therapy in patients with diabetes. The present study tried to find out whether compassion-focused therapy (CFT) and ABCT influence blood glucose level and medication adherence in diabetics or not.
Materials and Methods
This quasi-experimental study was conducted based on a pretest and posttest design with two experimental and one control groups. The statistical population of this research included a total number of 300 individuals with diabetes referred to
the Alborz Diabetes Association, Alborz, Iran. Regarding the sampling, at first, the researcher participated in the conferences of the Diabetes Association and delivered a speech about the goals and characteristics of the mentioned course and the inclusion criteria of this research project. Subsequently, the researcher collected the contact numbers of the volunteers.
Finally, 45 out of the 300 patients were invited to participate in the study through random assignment. The inclusion criteria in this study were 1) age range of 30-65 years, 2) minimum reading and writing ability, and 3) written confirmation of the disease by a qualified physician and based on the results of diagnostic tests. Moreover, the exclusion criteria were infliction with severe medical complications
of diabetes and consumption of psychotropic medication or medication abuse.
The first experimental group received 10 two-h sessions of CFT while the second group received eight two-and-half-h sessions of ABCT. It must be noted that the control group did not receive any intervention during this period. All participants were randomly assigned to three groups with equal numbers and written informed consent was obtained from the participants. In addition, pretest assessments were performed on all the participants.
Medication adherence scale (MAS)
Morisky's medication adherence questionnaire includes seven two-point options (Yes (0), No (1)) and one five-point option ranging from never (0) to always (4). A score of six or higher on this scale shows optimal medication adherence [20]. This questionnaire was translated into Persian for the first time by Bakaian [21] and its validity and reliability were confirmed. Reliability of this questionnaire was calculated at 0.89 by Cronbach's alpha coefficient.
Hemoglobin A1c Blood Test
The (Hemoglobin A1c) HbA1c is a protein that has been clinically recognized as the most important indicator of long-term blood control monitoring. This test measures the average blood glucose level for the preceding two to three months [22]. In fact, the effect of therapy and improvement in blood glucose control is manifested in HbA1c reduction [23]. This indicator is reported as a percentage and is interpretable based on the normal range which is specified by each laboratory.
First, a blood test was performed on the experimental groups; afterward, they were asked to complete a medication adherence questionnaire as well as a consent form for participation in this research. Subsequently, they underwent CFT and ABCT in group form during weekly sessions. The CFT included 10 sessions of self-compassion therapy based on the concepts of Gilbert (2010).
Attachment-based compassion therapy
This therapy includes eight two-and-half-hour sessions that include mindfulness and compassion training, such as receiving and offering love and compassion to friends, people who seem suspicious, strangers, and themselves. This program includes daily homework that lasts approximately 15-20 min. Moreover, it includes eight sessions as follows: 1) preparation of individuals for compassionate care with love, 2) discovery of the world of self-compassion, 3) development of a compassionate world, 4) comprehension of relationships with compassion, 5) development of one’s own self (the importance of love towards themselves and others), 6) advanced compassion 1 (forgiveness), 7) advanced compassion 2 (adaptation of the form of attachment and examination of different relationships), and 8) beyond compassion: sobriety and serenity.
At the end of the intervention program, the HbA1c levels of blood in all three groups were re-evaluated, and all individuals completed a post-test medication adherence questionnaire. Analysis of covariance was used to analyze the data and to determine the effectiveness of CFT training and ABCT on medication adherence and control of blood glucose in diabetic patients.
The collected data were analyzed in SPSS software (version 22) using descriptive statistical methods, such as mean, standard deviation, and analysis of Covariance. Moreover, Levene’s test was used to examine the assumption of variance equality of variables. In addition, the normality of distributing scores in the society was observed using the Skewness and Kurtosis tests.
Results
Based on the results, 10 (71%), 11 (73%), and 9 (60%) subjects in the first and second experimental, and control groups were female, respectively. It must be noted that each research group consisted of 15 participants. The mean, standard deviation, blood glucose levels, and medication adherence scores were calculated and the results are summarized in Table 1.
Based on Table 2, considering the intragroup factor, the calculated F value was significant for the effect of phases (i.e., pre-test, post-test, and follow-up) at a level smaller than 0.01 (Eta= 0.32, F=19.72, P<0.0001). As a result, there was a
Table 1. Mean and standard deviation of research variables
| Group | Variable | Pretest | Posttest | Follow-up | |||
| M | SD | M | SD | M | SD | ||
| Compassion-focused therapy | Blood glucose level | 7.9 | 1.3 | 7.2 | 1.2 | 7 | 1.2 |
| Medication adherence | 3 | 1.6 | 2.07 | 1.5 | 2.1 | 1.4 | |
| Attachment-based compassion therapy | Blood glucose level | 7.5 | 1.1 | 7.2 | 0.92 | 7.1 | 0.87 |
| Medication adherence | 3.2 | 1.7 | 2.4 | 1.4 | 2.3 | 1.3 | |
| Control group | Blood glucose level | 7.5 | 1.1 | 7.2 | 0.92 | 7.1 | 0.86 |
| Medication adherence | 3.8 | 2.1 | 4.1 | 1.6 | 3.9 | 1.7 | |
Table 2. Results of mixed analysis of variance with intragroup and intergroup factors regarding the blood glucose level variable
| Variables | Factors | Sources of change | sum of squares | Degrees of freedom | Mean squares | F | Significance | Eta |
| Blood glucose level | Intragroup factors | Time phases | 6.06 | 1.1 | 5.53 | 19.72 | 0.0001 | 0.32 |
| Interaction of phases*group | 3.15 | 2.2 | 1.44 | 5.13 | 0.008 | 0.20 | ||
| Intergroup factor | Group | 5.19 | 2 | 2.59 | 0.917 | 0.408 | 0.04 | |
| Error | 116.11 | 41 | 2.83 | |||||
| Medication adherence variable | Intragroup factors | Time phases | 8.45 | 1.2 | 6.88 | 6.45 | 0.01 | 0.136 |
| Interaction of phases*group | 7.407 | 2.4 | 3.01 | 2.826 | 0.03 | 0.121 | ||
| Intergroup factor | Group | 64.77 | 2 | 32.38 | 4.77 | 0.014 | 0.189 | |
| Error | 277.86 | 41 | 6.77 |
Table 3. Summary of Bonferroni Post-Hoc test results
| Phases/groups | Mean differences | Standard error | Sig. | |
| Phases | Pretest-posttest | 0.382* | 0.096 | 0.001 |
| Pretest-follow up | 0.503* | 0.105 | 0.0001 | |
| Pretest-follow up | 0.122* | 0.027 | 0.0001 | |
| Groups | Compassion-focused – attachment-based compassion therapy | 0.107 | 0.361 | 0.99 |
| Compassion-focused – control | - 0.353 | 0.361 | 0.99 | |
| Attachment-based compassion therapy – control | - 0.460 | 0.355 | 0.606 | |
| Phases | Pretest-posttest | 0.576* | 0.199 | 0.018 |
| Pretest-follow up | 0.487* | 0.208 | 0.043 | |
| Pretest-follow up | 0.089* | 0.079 | 0.807 | |
| Groups | Compassion-focused – attachment-based compassion therapy | - 0.263 | 0.559 | 0.99 |
| Compassion-focused – control | - 1.59* | 0.559 | 0.02 | |
| Attachment-based compassion therapy – control | - 1.33 | 0.549 | 0.059 |
*P<0.05
significant difference between the mean scores of blood glucose levels of the three groups during the pretest, posttest, and follow-up stages. Moreover, regarding the intergroup factor, the calculated F value at the level of 0.05 was not significant (Eta=0.043, P>0.05, F=0.91). Therefore, there was no significant difference between the total mean blood glucose level in the experimental and control groups.
Given the intragroup factor, the calculated F value was significant for the effect of stages (i.e., pretest, posttest, and follow-up) at a level less than 0.01 (Eta=0.136, P<0.01, F=6.45). Therefore, there was a significant difference between the mean scores of medication adherence in the three groups during the pretest, posttest, and follow-up stages. Besides, the calculated F value (0.05) was significant for the intergroup factor (Eta=0.189, P<0.05, F=4.77). As a result, there was a significant difference between the total mean value of medication adherence in the three experimental and control groups. The Bonferroni post-hoc test was performed to examine the difference between the means. The results are shown in Table 3.
Generally, it can be concluded that in the first experimental group, CFT was significantly effective in increasing medication adherence in diabetic patients, and this therapy has an enduring effect over the course of time (figures 1 and 2).
Given the intragroup factor, the calculated F value was significant for the effect of stages (i.e., pretest, posttest, and follow-up) at a level less than 0.01 (Eta=0.136, P<0.01, F=6.45). Therefore, there was a significant difference between the mean scores of medication adherence in the three groups during the pretest, posttest, and follow-up stages. Besides, the calculated F value (0.05) was significant for the intergroup factor (Eta=0.189, P<0.05, F=4.77). As a result, there was a significant difference between the total mean value of medication adherence in the three experimental and control groups. The Bonferroni post-hoc test was performed to examine the difference between the means. The results are shown in Table 3.
Generally, it can be concluded that in the first experimental group, CFT was significantly effective in increasing medication adherence in diabetic patients, and this therapy has an enduring effect over the course of time (figures 1 and 2).

Figure 1. Adjusted means of blood glucose level in both experimental and control groups during the studied phases
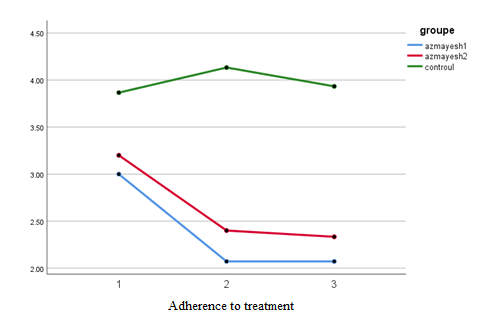
Figure 2. Adjusted means of medication adherence scores in both experimental and control groups during the studied phases
Discussion
This study aimed to investigate the effectiveness of CFT and ABCT interventions on the control of blood glucose level (HbA1c) and medication adherence in diabetic patients. Based on the results, CFT and ABCT interventions had a significant effect on the improvement of blood glucose control and promotion of medication adherence in patients with diabetes.
It must be mentioned that no previous research had been performed about the effectiveness of these therapeutic interventions on the process of medication adherence and blood glucose control of diabetic patients. Nevertheless, it can be said that the findings of this study are somewhat in line with those of some previous studies carried out by Attari et al. [24] and Mehrabi et al. [25] on type 1 diabetic patients and Suruit et al. [26] and Dawazdah Emami et al. [27] on type 2 diabetic patients.
Since self-compassion helps many individuals to cope with their life problems, it should be noted that self-compassion does not reject negative emotions altogether. Through self-compassion we can create positive emotions in ourselves by accepting negative emotions and manipulating them rather than substituting them with positive ones. Indeed, self-compassion is associated with higher mental powers needed for survival, such as happiness, optimism, alertness, curiosity, exploration, personal initiatives, and emotional awareness.
Self-compassionate people do not fear failure and are able to strive for success over and over again after each failure [28]. Bernice and Chen [29] found that self-compassion for previous personal weaknesses, failures, and moral problems cause individuals to have a higher motivation for change, try to learn more, and not repeat their past mistakes.
In the same way, self-compassion also increases the motivation regarding health and wellness issues, such as medication adherence and continuation of diet and nutrition regimen. Self-compassion is also associated with altruism, responsibility, and forgiving of others [30] which can help control the blood glucose level and increase medication adherence in diabetic patients [31]. Other studies have suggested that self-compassion is associated with attachment systems. Self-compassion leads to modification of interpersonal relationships and the resulting disorders which, in turn, leads to an increased level of acceptance and medication adherence in diabetic patients [32].
Self-compassion strategies and secure attachment used in this study included preparation of individuals for compassionate care, discovery and development of a compassionate world, adaptation of attachments and examination of relationships, calmness and serenity, absorbance of self-compassion from others, display self-compassion to others, and face its psychological consequences in a more logical way [33].
The subjects used their acquired skills to improve themselves and control their disease in an effective manner. Such a belief plays a significant role in the maintenance of one’s mental health since being worried about high blood glucose and its consequences as well as a negative attitude towards therapy have harmful consequences. They can lead to a lot of mental energy consumption and in many cases can cause self-criticism, self-blame, frustration, a sense of failure, and mental rumination in the patient [34].
Furthermore, in this intervention, emotion regulation systems were managed; accordingly, the threat system activation was reduced, while the relief system activation was increased. For this purpose, negative emotions, including anxiety, anger, hatred, and behaviors, such as war-mongering and surrendering before this disease, were reduced and patients felt safe and healthy in their minds [35].
Conclusions
The CFT and ABCT can be effective in the improvement of medication adherence and blood glucose control (HbA1c) in diabetic patients. Therefore, it is suggested to provide such training together with other medical interventions as part of a comprehensive therapy of diabetes.
Compliance with ethical guidelines
All ethical principles were considered in this research. In this regard, the participants were informed about the purpose of the research and its stages, and informed consent was obtained from them. They were also assured of the confidentiality of their information. Moreover, the subjects were free to withdraw from the study at any time. They were also informed that they would be provided with the results of the research. This research has an ethical code (IR.IAU.TON.REC.1398.025) from the Islamic Azad University, Tonekabon Branch, Tonekabon, Iran.
Acknowledgments
The authors would like to thank the participants who greatly cooperated with them in this research project.
Authorsʼ contributions
Conceptualization: Mansoreh Yazdani; methodology: Javad Khalatbari; investigation: Mehri Raoufi; preparation of the original draft: Shohreh Ghorban Shiroudi; writing of the article and affiliation, reviewing, and editing: Mohammad Ali Rahmani; funding acquisition: all authors; references: all author; supervision: Javad Khalatbari.
Funding/Support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare that there was no conflict of interest in this study.
References
This study aimed to investigate the effectiveness of CFT and ABCT interventions on the control of blood glucose level (HbA1c) and medication adherence in diabetic patients. Based on the results, CFT and ABCT interventions had a significant effect on the improvement of blood glucose control and promotion of medication adherence in patients with diabetes.
It must be mentioned that no previous research had been performed about the effectiveness of these therapeutic interventions on the process of medication adherence and blood glucose control of diabetic patients. Nevertheless, it can be said that the findings of this study are somewhat in line with those of some previous studies carried out by Attari et al. [24] and Mehrabi et al. [25] on type 1 diabetic patients and Suruit et al. [26] and Dawazdah Emami et al. [27] on type 2 diabetic patients.
Since self-compassion helps many individuals to cope with their life problems, it should be noted that self-compassion does not reject negative emotions altogether. Through self-compassion we can create positive emotions in ourselves by accepting negative emotions and manipulating them rather than substituting them with positive ones. Indeed, self-compassion is associated with higher mental powers needed for survival, such as happiness, optimism, alertness, curiosity, exploration, personal initiatives, and emotional awareness.
Self-compassionate people do not fear failure and are able to strive for success over and over again after each failure [28]. Bernice and Chen [29] found that self-compassion for previous personal weaknesses, failures, and moral problems cause individuals to have a higher motivation for change, try to learn more, and not repeat their past mistakes.
In the same way, self-compassion also increases the motivation regarding health and wellness issues, such as medication adherence and continuation of diet and nutrition regimen. Self-compassion is also associated with altruism, responsibility, and forgiving of others [30] which can help control the blood glucose level and increase medication adherence in diabetic patients [31]. Other studies have suggested that self-compassion is associated with attachment systems. Self-compassion leads to modification of interpersonal relationships and the resulting disorders which, in turn, leads to an increased level of acceptance and medication adherence in diabetic patients [32].
Self-compassion strategies and secure attachment used in this study included preparation of individuals for compassionate care, discovery and development of a compassionate world, adaptation of attachments and examination of relationships, calmness and serenity, absorbance of self-compassion from others, display self-compassion to others, and face its psychological consequences in a more logical way [33].
The subjects used their acquired skills to improve themselves and control their disease in an effective manner. Such a belief plays a significant role in the maintenance of one’s mental health since being worried about high blood glucose and its consequences as well as a negative attitude towards therapy have harmful consequences. They can lead to a lot of mental energy consumption and in many cases can cause self-criticism, self-blame, frustration, a sense of failure, and mental rumination in the patient [34].
Furthermore, in this intervention, emotion regulation systems were managed; accordingly, the threat system activation was reduced, while the relief system activation was increased. For this purpose, negative emotions, including anxiety, anger, hatred, and behaviors, such as war-mongering and surrendering before this disease, were reduced and patients felt safe and healthy in their minds [35].
Conclusions
The CFT and ABCT can be effective in the improvement of medication adherence and blood glucose control (HbA1c) in diabetic patients. Therefore, it is suggested to provide such training together with other medical interventions as part of a comprehensive therapy of diabetes.
Compliance with ethical guidelines
All ethical principles were considered in this research. In this regard, the participants were informed about the purpose of the research and its stages, and informed consent was obtained from them. They were also assured of the confidentiality of their information. Moreover, the subjects were free to withdraw from the study at any time. They were also informed that they would be provided with the results of the research. This research has an ethical code (IR.IAU.TON.REC.1398.025) from the Islamic Azad University, Tonekabon Branch, Tonekabon, Iran.
Acknowledgments
The authors would like to thank the participants who greatly cooperated with them in this research project.
Authorsʼ contributions
Conceptualization: Mansoreh Yazdani; methodology: Javad Khalatbari; investigation: Mehri Raoufi; preparation of the original draft: Shohreh Ghorban Shiroudi; writing of the article and affiliation, reviewing, and editing: Mohammad Ali Rahmani; funding acquisition: all authors; references: all author; supervision: Javad Khalatbari.
Funding/Support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare that there was no conflict of interest in this study.
References
- Al-Qasem A, Smith F, Clifford S. Adherence to medication among chronic patients in Middle Eastern countries: review of studies. Eastern Mediterranean Health Journal. 2011; 17(4):356-63. [DOI:10.26719/2011.17.4.356] [PMID]
- Alfian SD, Sukandar H, Lestari K, Abdulah R. Medication adherence contributes to an improved quality of life in type 2 diabetes mellitus patients: a cross-sectional study. Diabetes Therapy. 2016; 7(4):755-64. [DOI:10.1007/s133
00-016-0203-x] [PMID] [PMCID] - Al-Qazaz HK, Sulaiman SA, Hassali MA, Shafie AA, Sundram S, Al-Nuri R, et al. Diabetes knowledge, medication adherence and glycemic control among patients with type 2 diabetes. International Journal of Clinical Pharmacy. 2011; 33(6):1028-35. [DOI:10.1007/s11096-011-9582-2] [PMID]
- Atinga RA, Yarney L, Gavu NM. Factors influencing long-term medication non-adherence among diabetes and hypertensive patients in Ghana: a qualitative investigation. PLoS One. 2018; 13(3):e0193995. [DOI:10.1371/journal.pone.0193995] [PMID] [PMCID]
- Bakar ZA, Fahrni ML, Khan TM. Patient satisfaction and medication adherence assessment amongst patients at the diabetes medication therapy adherence clinic. Diabetes & Metabolic Syndrome. 2016; 10(2 Suppl 1):S139-43. [DOI:10.1016/j.dsx.2016.03.015] [PMID]
- Bitton A, Choudhry NK, Matlin OS, Swanton K, Shrank WH. The impact of medication adherence on coronary artery disease costs and outcomes: a systematic review. The American Journal of Medicine. 2013; 126(4):357.e7-27. [DOI:10.1016/j.amjmed.2012.09.004] [PMID]
- Brummel A, Carlson AM. Comprehensive medication management and medication adherence for chronic conditions. Journal of Managed Care & Specialty Pharmacy. 2016; 22(1):56-62. [DOI:10.18553/jmcp.2016.22.1.56] [PMID]
- Cani CG, Da Silva Girão Lopes L, Queiroz M, Nery M. Improvement in medication adherence and selfmanagement of diabetes with a clinical pharmacy program: a randomized controlled trial in patients with type 2 diabetes undergoing insulin therapy at a teaching hospital. Clinics. 2015; 70(2):102-6. [DOI:10.6061/clinics/2015(02)06] [PMID] [PMCID]
- Erku DA, Ayele AA, Mekuria AB, Belachew SA, Hailemeskel B, Tegegn HG. The impact of pharmacist-led medication therapy management on medication adherence in patients with type 2 diabetes mellitus: a randomized controlled
study. Pharmacy Practice (Granada). 2017; 15(3):1026. [DOI:10.18549/PharmPract.2017.03.1026] [PMID] [PMCID] - Farsaei S, Radfar M, Heydari Z, Abbasi F, Qorbani M. Insulin adherence in patients with diabetes: risk factors for injection omission. Primary Care Diabetes. 2014; 8(4):338-45. [DOI:10.1016/j.pcd.2014.03.001] [PMID]
- Fischer MA, Stedman MR, Lii J, Vogeli C, Shrank WH, Brookhart MA, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. Journal
of General Internal Medicine. 2010; 25(4):284-90. [DOI:10.1007/s11606-010-1253-9] [PMID] [PMCID] - Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: How unintentional is it really? BMC Health Services Research. 2012; 12(1):98. [DOI:10.1186/1472-6963-12-98] [PMID] [PMCID]
- García-Pérez LE, Álvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Therapy. 2013; 4(1):175-94. [DOI:10.1007/s13300-013-0034-y] [PMID] [PMCID]
- Ghimire S, Castelino RL, Lioufas NM, Peterson GM, Zaidi STR. Nonadherence to medication therapy in haemodialysis patients: a systematic review. PLoS One. 2015; 10(12):
e0144119. [DOI:10.1371/journal.pone.0144119] [PMID] [PMCID] - Gonzalez JS, Shreck E, Psaros C, Safren SA. Distress and type 2 diabetes-treatment adherence: a mediating role for perceived control. Health Psychology. 2015; 34(5):505-13. [DOI:10.1037/hea0000131] [PMID] [PMCID]
- Gwadry-Sridhar FH, Manias E, Lal L, Salas M, Hughes DA, Ratzki-Leewing A, et al. Impact of interventions on medication adherence and blood pressure control in patients with essential hypertension: a systematic review by the ISPOR medication adherence and persistence special interest group. Value in Health. 2013; 10(2):863-71. [DOI:10.1016/j.jval.2013.03.1631] [PMID]
- Hall AK, Cole-Lewis H, Bernhardt JM. Mobile text messaging for health: a systematic review of reviews. Annual Review of Public Health. 2015; 36(1):393-415. [DOI:10.1146/annurev-publhealth-031914-122855] [PMID] [PMCID]
- Islam SM, Lechner A, Ferrari U, Froeschl G, Alam DS, Holle R, et al. Mobile phone intervention for increasing adherence to treatment for type 2 diabetes in an urban area
of Bangladesh: Protocol for a randomized controlled
trial. BMC Health Services Research. 2014; 14(1):589. [DOI:10.1186/s12913-014-0586-1] [PMID] [PMCID] - Iuga AO, McGuire MJ. Adherence and health care costs. Risk Management and Healthcare Policy. 2014; 7:35-44. [DOI:10.2147/RMHP.S19801] [PMID] [PMCID]
- Katz LL, Anderson BJ, McKay SV, Izquierdo R, Casey TL, Higgins LA, et al. Correlates of medication adherence in the TODAY cohort of youth with type 2 diabetes. Diabetes Care. 2016; 39(11):1956-62. [DOI:10.2337/dc15-2296] [PMID] [PMCID]
- Kirkman MS, Rowan-Martin MT, Levin R, Fonseca VA,
Schmittdiel JA, Herman WH, et al. Determinants of adherence to diabetes medications: findings from a large pharmacy claims database. Diabetes Care. 2015; 38(4):604-9. [DOI:10.2337/dc14-2098] [PMID] [PMCID] - Lim PC, Lim K. Evaluation of a pharmacist-managed diabetes medication therapy adherence clinic. Pharmacy Practice (Granada). 2010; 8(4):250-4. [DOI:10.4321/S1886-36552010000400008] [PMID] [PMCID]
- Lin LK, Sun Y, Heng BH, Kwang Chew DE, Chong PN. Medication adherence and glycemic control among newly diagnosed diabetes patients. BMJ Open Diabetes Research & Care. 2017; 5(1):e000429. [DOI:10.1136/bmjdrc-2017-000429] [PMID] [PMCID]
- Mann DM, Ponieman D, Leventhal H, Halm EA. Predictors of adherence to diabetes medications: The role of disease and medication beliefs. Journal of Behavioral Medicine. 2009; 32(3):278-84. [DOI:10.1007/s10865-009-9202-y] [PMID]
- Marzec LN, Maddox TM. Medication adherence in patients with diabetes and dyslipidemia: Associated factors and strategies for improvement. Current Cardiology Reports. 2013; 15(11):418. [DOI:10.1007/s11886-013-0418-7] [PMID]
- Monroe AK, Pena JS, Moore RD, Riekert KA, Eakin MN, Kripalani S, et al. Randomized controlled trial of a pictorial aid intervention for medication adherence among HIV-positive patients with comorbid diabetes or hypertension. AIDS Care. 2018; 30(2):199-206. [DOI:10.1080/09540121.
2017.1360993] [PMID] - Reeder B, David A. Health at hand: a systematic review of smart watch uses for health and wellness. Journal of Biomedical Informatics. 2016; 63:269-76. [DOI:10.1016/
j.jbi.2016.09.001] [PMID] - Safren SA, Gonzalez JS, Wexler DJ, Psaros C, Delahanty LM, Blashill AJ, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in patients with uncontrolled type 2 diabetes. Diabetes Care. 2014; 37(3):625-33. [DOI:10.2337/dc13-0816] [PMID] [PMCID]
- Sapkota S, Brien JA, Greenfield J, Aslani P. A systematic review of interventions addressing adherence to anti-diabetic medications in patients with type 2 diabetes -- impact on adherence. PLoS One. 2015; 10(2):e118296. [DOI:10.1371/journal.pone.0118296] [PMID] [PMCID]
- Sarbacker GB, Urteaga EM. Adherence to insulin therapy. Diabetes Spectrum. 2016; 29(3):166-70. [DOI:10.2337/
diaspect.29.3.166] [PMID] [PMCID] - Skinta MD, Lezama M, Wells G, Dilley JW. Acceptance and compassion-based group therapy to reduce HIV stigma. Cognitive and Behavioral Practice. 2015; 22(4):481-90. [DOI:10.1016/j.cbpra.2014.05.006]
- Sontakke S, Jadhav M, Pimpalkhute S, Jaiswal K, Bajait C. Evaluation of adherence to therapy in patients of type 2 diabetes mellitus. Journal of Young Pharmacists. 2015; 7(4):462-9. [DOI:10.5530/jyp.2015.4s.8]
- Tiv M, Viel JF, Mauny F, Eschwège E, Weill A, Fournier C, et al. Medication adherence in type 2 diabetes: the ENTRED study 2007, a French population-based study. PLoS One. 2012; 7(3):e32412. [DOI:10.1371/journal.pone.0032412] [PMID] [PMCID]
- Wabe NT, Angamo MT, Hussein S. Medication adherence in diabetes mellitus and self management practices among type-2 diabetics in Ethiopia. North American Journal
of Medical Sciences. 2011; 3(9):418-23. [DOI:10.4297/
najms.2011.3418] [PMID] [PMCID] - Wolever RQ, Dreusicke M, Fikkan J, Hawkins TV, Yeung S, Wakefield J, et al. Integrative health coaching for patients with type 2 diabetes: a randomized clinical trial. The Diabetes Educator. 2010; 36(4):629-39. [DOI:10.1177/
0145721710371523] [PMID]
Article Type: Research Article |
Subject:
Health Education and Promotion
Received: 2020/06/4 | Accepted: 2020/07/31 | Published: 2021/02/2
Received: 2020/06/4 | Accepted: 2020/07/31 | Published: 2021/02/2
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |